Every year, thousands of people end up in the hospital not because of a fall, a car accident, or a bad flu - but because they took a common pain reliever the wrong way. You probably have it in your medicine cabinet right now: acetaminophen. It’s in Tylenol, in cold medicines, in sleep aids, and in dozens of other products you might not even realize contain it. And while it’s safe when used correctly, taking too much - even just a little too much - can cause serious, sometimes deadly, liver damage.
Why Acetaminophen Is a Silent Threat
Acetaminophen is one of the most widely used pain relievers in the world. It’s in over 600 different medications, both prescription and over-the-counter. That means if you take a cold medicine, a headache pill, and a sleep aid on the same day, you could be hitting your liver with three separate doses - without ever realizing it.
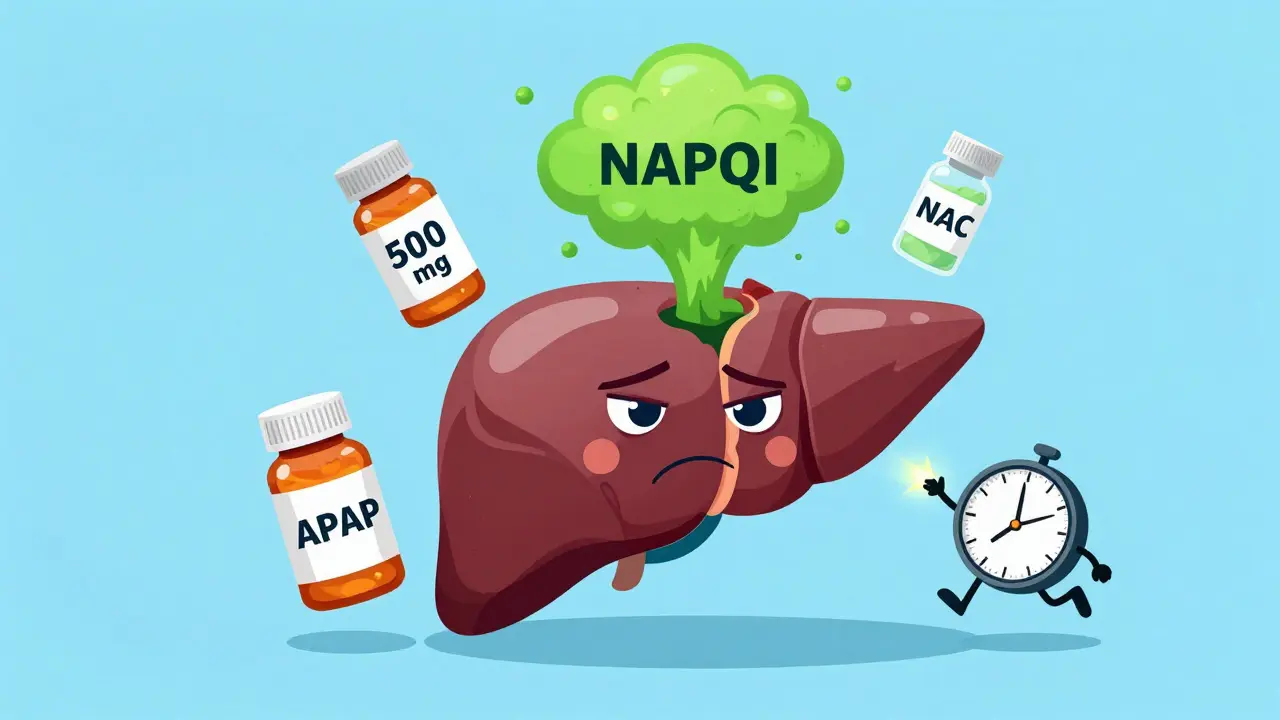
The problem isn’t the drug itself. At normal doses, acetaminophen is broken down safely by the liver. But when you take too much, your liver runs out of a natural protective chemical called glutathione. Without it, a toxic byproduct called NAPQI builds up and starts killing liver cells. This isn’t a slow process. Damage can start within hours, and symptoms often don’t show up until it’s too late.
In the U.S., acetaminophen is the leading cause of acute liver failure. According to CDC data from 2023, it causes about 56,000 emergency room visits, 26,000 hospital stays, and nearly 500 deaths every year. And here’s the scary part: 30 to 50% of those cases are unintentional. People didn’t mean to overdose. They just didn’t know how much they were taking.
What’s a Safe Dose? It Depends on You
The old rule was: don’t take more than 4,000 mg in one day. That’s eight 500 mg pills. But that number isn’t safe for everyone anymore.
- Healthy adults: The FDA now recommends a maximum of 3,250 mg per day for prescription combinations, and many experts advise staying under 3,000 mg even for OTC use.
- People with liver disease: If you have hepatitis, fatty liver, cirrhosis, or even just a history of heavy drinking, your limit is 2,000 mg per day - no more.
- People who drink alcohol: Even one drink a day can make your liver more vulnerable. If you drink regularly, your safe limit drops to 2,000 mg or less. Alcohol and acetaminophen together create a dangerous combo that can cause liver injury at doses you’d normally think are harmless.
And don’t forget: one extra-strength Tylenol tablet is 500 mg. So if you take two every four hours, you’re already at 3,000 mg in a day. Add a cold medicine with acetaminophen? You’re over the edge.
Hidden Sources of Acetaminophen
Most people think they’re safe if they’re only taking Tylenol. But here’s where things get tricky.
More than 25% of unintentional overdoses happen because people take cold, flu, or sleep medicines that contain acetaminophen - and they don’t check the label. Products like NyQuil, Excedrin, Theraflu, and even some allergy or sinus remedies list acetaminophen as an ingredient. If you’re taking more than one OTC product at a time, you’re likely doubling up.
Here’s how to avoid this:
- Always read the “Active Ingredients” section on the label.
- Look for “acetaminophen,” “APAP,” or “paracetamol.”
- If you’re unsure, ask a pharmacist. They’re trained to catch these overlaps.
- Use a pill organizer with daily dose reminders - especially if you take multiple meds.
There’s a reason the FDA now requires all OTC acetaminophen products to have a bold “Liver Warning” on the front. It’s because people keep missing it.
NSAIDs: A Different Kind of Risk
Not all pain relievers are created equal. Ibuprofen (Advil, Motrin) and naproxen (Aleve) are NSAIDs - they work differently than acetaminophen. They don’t directly damage the liver the same way. But they come with their own dangers.
NSAIDs are harder on your stomach and kidneys. They can cause ulcers, bleeding, and kidney damage, especially if you take them daily for long periods. Diclofenac, in particular, has been linked to rare but serious liver injury, according to FDA adverse event reports from 2023.
So if you have liver disease, NSAIDs aren’t automatically safer. The American Liver Foundation and Veterans Affairs guidelines both say: avoid NSAIDs in advanced liver disease because they can worsen kidney function and cause fluid retention - both dangerous if your liver is already struggling.
For people with liver conditions, acetaminophen (at low doses) is still the preferred option - as long as you stick to the limits. NSAIDs are riskier overall for this group.
What to Do If You Think You’ve Taken Too Much
Symptoms of liver injury from acetaminophen don’t show up right away. You might feel fine for 24 to 48 hours. Then, suddenly, you get nauseous, dizzy, or start feeling pain in the upper right side of your belly. Your urine turns dark. Your skin or eyes look yellow. That’s jaundice - a red flag.
If you suspect you’ve taken too much - even if you feel fine - don’t wait. Call Poison Control (1-800-222-1222 in the U.S.) or go to the ER immediately. The antidote, N-acetylcysteine (NAC), works best if given within 8 hours of overdose. After 16 hours, it’s much less effective.
Don’t try to “wait it out.” Liver damage from acetaminophen can progress rapidly. By the time you feel sick, your liver may already be failing.
Smart Alternatives for Chronic Pain
If you’re dealing with ongoing pain - back pain, arthritis, headaches - relying on daily pills isn’t the answer. The American Liver Foundation now recommends non-drug approaches as first-line treatments:
- Physical therapy
- Cognitive behavioral therapy (CBT) for pain management
- Acupuncture
- Heat or cold therapy
- Topical NSAIDs (gels or patches) - these don’t enter your bloodstream the same way as pills, so they’re much safer for your liver
For occasional pain, try using the lowest effective dose for the shortest time. Don’t use pain relievers as a daily habit unless your doctor says so.
Protecting Your Liver: A Simple Checklist
Here’s what you can do right now to protect your liver:
- Know your daily limit: 2,000 mg if you have liver issues or drink alcohol; 3,000 mg max if you’re healthy.
- Check every medicine label - even vitamins and supplements.
- Never mix acetaminophen with alcohol.
- Wait at least 8 hours between doses.
- Use a pill organizer with daily max markers.
- Keep a written log of all medications you take, including OTC ones.
- Ask your pharmacist to review your meds if you take more than five different ones.
- Consider non-drug pain relief before reaching for pills.
There’s no shame in asking for help. Pharmacists are there to catch these mistakes before they happen. And if you’re managing chronic pain, talk to your doctor about safer long-term strategies.
Future Trends: Safer Pain Relief on the Horizon
Researchers are working on new pain medications that don’t go through the liver at all. The NIH has allocated $47 million toward developing analgesics with minimal liver metabolism. Some companies are even exploring genetic testing - like 23andMe - to identify people who naturally process acetaminophen poorly and need lower doses.
For now, the best defense is knowledge. You don’t need to avoid acetaminophen. You just need to use it wisely.


Niel Amstrong Stein
February 7, 2026 AT 13:51