Why Your Medications Expire Sooner Than They Should
Most people think expiration dates are just printed on the bottle to scare them into buying new medicine. But here’s the truth: if you store your pills, liquids, or patches wrong, they can lose their strength long before that date. In fact, the CDC says nearly 4 out of 10 cases of early expiration happen because of how people store them at home - not because the drug itself is bad.
Imagine taking a painkiller that’s lost 30% of its power because it sat above the toilet. Or insulin that turned useless after a summer heatwave. These aren’t hypotheticals. They happen every day. And the cost? Over $20 billion a year in the U.S. alone gets thrown away because meds degrade in bad conditions.
The Storage Rules No One Tells You
The FDA says a medication’s expiration date means it’s guaranteed to work as labeled only if stored correctly. That’s the key. Most drugs are tested to stay strong at room temperature: between 20°C and 25°C (68°F-77°F). But that doesn’t mean your bathroom cabinet is fine.
Here’s what actually works:
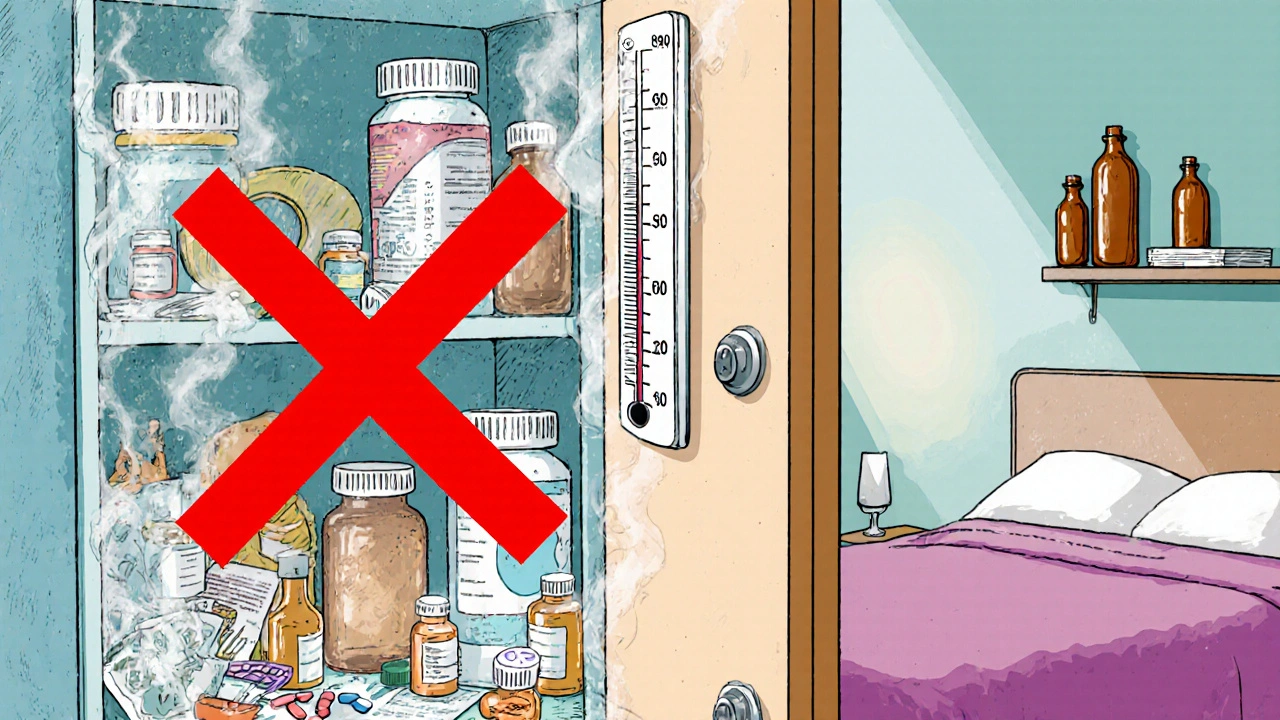
- Keep meds away from humidity. Bathrooms are the worst place. Showers spike humidity to 85-95%. Aspirin breaks down 3 times faster in that kind of moisture. The same goes for antibiotics, thyroid pills, and antidepressants.
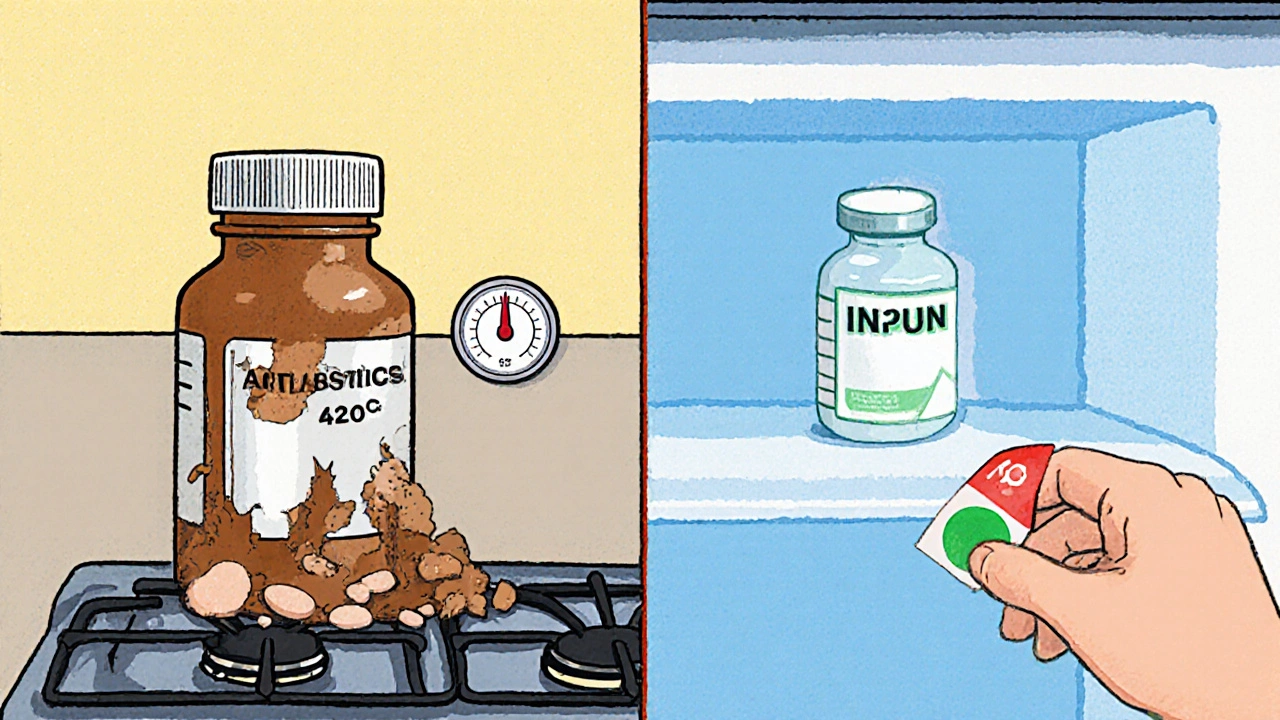
- Avoid heat sources. Kitchens are risky too. Stoves, ovens, and even dishwashers create temperature swings. One study found 42% of common antibiotics lost potency within 90 days when stored near the stove.
- Use the original container. Those amber bottles aren’t just for looks. They block 97% of UV light, which can break down medications like nitroglycerin and certain antibiotics. Transfer pills to a pill organizer? Fine - but keep the original bottle in a cool, dry spot.
- Don’t store in drawers unless they’re climate-controlled. Dresser drawers are better than bathrooms, but only if they’re not in a hot room. The ideal spot? A bedroom shelf, away from windows, near the floor (heat rises).
What About the Fridge?
Not all meds need refrigeration - but the ones that do, really need it.
Insulin, certain antibiotics, eye drops, and liquid suspensions often require 2°C to 8°C (36°F-46°F). But don’t just toss them in the fridge door. That’s the warmest part. Put them in the center, where the temperature stays steady. Use a small fridge thermometer to check. If it’s above 8°C, your insulin could be losing strength.
And here’s a trick: once you open insulin, you can keep it at room temperature for up to 28 days. No need to keep chilling it. Just write the date you opened it on the bottle. Same goes for some eye drops - check the label.
Special Cases: What’s Different?
Some meds have unique needs. Ignore them, and you risk serious problems.
- Nitroglycerin (for chest pain): Must stay in its original glass bottle. It’s so sensitive to light and air that even a new plastic container can ruin it. Keep it tightly closed and away from heat.
- Epinephrine auto-injectors (EpiPens): Don’t freeze them. Don’t leave them in a hot car. Store at room temperature, but check the color. If it turns brown or cloudy, replace it - even if it’s not expired.
- Suppositories and creams: These can melt. Store them in the fridge if the label says so. If they look oily or separated, toss them.
How to Spot Degraded Medication
You don’t need a lab to tell if your medicine is bad. Here’s what to look for:
- Smell: Aspirin that smells like vinegar? That’s acetylsalicylic acid breaking down. Don’t take it.
- Color: Tablets or capsules that changed color - especially darkened or spotted - are suspect. Even a 15% shift from the original hue is a red flag.
- Texture: Pills that crumble, stick together, or feel sticky? That’s moisture damage. Liquids with floating particles, cloudiness, or separation? Throw them out.
- Expiration date passed: Yes, some meds last longer. But the FDA says that’s only true for perfectly stored military stockpiles. At home? Don’t risk it.
Organize to Avoid Waste
Most people don’t check their meds until they need them. That’s how expired pills pile up.
Try this simple system:
- Find one spot - a locked cabinet in your bedroom or closet - that stays between 19°C and 22°C. Use a small hygrometer (under $15 online) to monitor humidity. Keep it below 60%.
- Group all meds there. No more scattered bottles in the bathroom, kitchen, or car.
- Use color-coded stickers: red for this year, blue for next, green for two years out. Update them every January.
- Assign one person in the household to do a monthly check. Look at dates. Check for changes. Toss anything questionable.
Studies show this cuts expired meds by over 60%. One hospital system reduced waste by 89% just by having someone check monthly.
What About Smart Tech?
There are gadgets now that help. Smart pillboxes like MedMinder Pro track temperature and humidity inside the box. If it gets too hot or humid, it sends a phone alert. They’re not cheap - around $150 - but if you take multiple critical meds, they’re worth it.
Also, more drug labels now include icons: a snowflake for refrigeration, a sun with a line through it for avoiding light, a house with a drop for avoiding moisture. Look for them.
And there’s new tech coming: bottles with built-in silica gel to control humidity. Trials show they reduce moisture exposure by 45%. They’ll be on shelves by late 2025.
What to Do With Expired or Unused Meds
Never flush them. Don’t throw them in the trash where kids or pets can get them. Don’t give them to friends.
Use a drug take-back program. In the U.S., the DEA runs National Prescription Drug Take Back Day twice a year. There are over 11,000 drop-off sites - pharmacies, police stations, hospitals. Find one near you at dea.gov/takebackday.
If there’s no event nearby, mix pills with coffee grounds or cat litter in a sealed bag. Throw it in the trash. It’s not perfect, but it’s safer than flushing.
Why This Matters Beyond Saving Money
It’s not just about wasting money. Taking degraded medication can be dangerous. Weak antibiotics won’t kill an infection - they might make it worse. Expired epinephrine might not stop an allergic reaction. A child taking a crumbling asthma inhaler could end up in the ER.
And it’s worse in rural areas. A 2024 study found 64% of rural households don’t have climate-controlled storage. Their meds degrade 41% faster than in cities. This isn’t a first-world problem - it’s a public health gap.
What’s Changing Soon
The FDA is pushing for real-time stability indicators on high-risk meds by 2025. Think color-changing strips on the bottle that show if the drug’s been exposed to heat or moisture. That could be a game-changer.
Meanwhile, companies like Merck are developing heat-stable insulin that lasts 56 days at 30°C. That’s huge for people without reliable refrigeration.
But until then, the best tool you have is knowledge. Store your meds right. Check them often. Toss what’s questionable. Your body - and your wallet - will thank you.
Can I still use medicine after the expiration date?
The expiration date is the last day the manufacturer guarantees full strength and safety - if stored correctly. Some medications, especially in perfect conditions, may still work after that date. But at home, where temperatures and humidity vary, it’s not safe to assume. Pills that look or smell off should be thrown out. Never use expired insulin, epinephrine, antibiotics, or liquid medications.
Is the bathroom medicine cabinet really that bad?
Yes. Showers create humidity levels of 85-95%, which causes pills to break down faster. Aspirin degrades 300% quicker in that environment. Heat from hair dryers and steam also raises the temperature. The CDC lists bathroom storage as one of the top causes of premature expiration. Keep meds in a cool, dry place like a bedroom drawer or cabinet instead.
Should I refrigerate all my medications?
No. Only refrigerate what the label says. Most tablets and capsules are fine at room temperature. Refrigerating them can cause moisture buildup inside the bottle, especially if you take them in and out often. Insulin, eye drops, and some antibiotics need cold storage. Always check the label or ask your pharmacist.
How do I know if my insulin is still good?
Check the color and clarity. Clear insulin should look like water. If it’s cloudy, clumpy, or has particles, don’t use it. Also, if it’s been left unrefrigerated for more than 28 days after opening, or if the expiration date has passed, replace it. Write the opening date on the bottle to track it.
What’s the best way to dispose of old meds?
Use a drug take-back program. The DEA hosts events twice a year at pharmacies, hospitals, and police stations. If there’s no event, mix pills with coffee grounds or cat litter in a sealed plastic bag and throw them in the trash. Never flush them - they pollute water systems and can harm wildlife.
Can I store medications in my car?
No. Cars get extremely hot in summer - over 50°C (120°F) - and freezing cold in winter. That kind of temperature swing destroys most medications. Even a few hours in a hot car can ruin insulin, epinephrine, or heart medications. Keep them with you indoors.
Are generic medications less stable than brand-name ones?
No. Generic drugs must meet the same FDA standards for strength, purity, and stability as brand-name versions. Their expiration dates are based on the same testing. The difference is cost, not quality. Store generics the same way you store brand-name meds.

Neoma Geoghegan
November 24, 2025 AT 20:14Bartholemy Tuite
November 25, 2025 AT 16:27Sam Jepsen
November 27, 2025 AT 01:29Yvonne Franklin
November 27, 2025 AT 20:15Patrick Marsh
November 29, 2025 AT 00:34Miruna Alexandru
November 30, 2025 AT 20:20Justin Daniel
December 1, 2025 AT 05:45Melvina Zelee
December 2, 2025 AT 01:28ann smith
December 2, 2025 AT 23:42Julie Pulvino
December 4, 2025 AT 14:24