Steroid Taper Duration Calculator
How Long Will Recovery Take?
Based on clinical guidelines, your recovery timeline depends on how long you were on steroids.
Your Estimated Recovery Timeline
When you’ve been on steroids for months or years, stopping them isn’t as simple as skipping a pill. Your body forgets how to make its own cortisol. If you quit too fast, you could end up in the hospital with an adrenal crisis-low blood pressure, vomiting, confusion, even collapse. That’s why steroid taper plans backed by ACTH stimulation testing have become the gold standard for safe recovery.
Why Your Adrenals Shut Down
When you take glucocorticoids like prednisone or hydrocortisone for more than a few weeks, your brain stops signaling your adrenal glands to produce cortisol. It’s not laziness-it’s biology. Your hypothalamus and pituitary gland think, “We’ve got plenty from outside, no need to work.” Over time, your adrenal glands shrink. They lose their ability to respond to stress. This isn’t rare. About 12.7% of people who stop long-term steroids without a proper plan develop adrenal insufficiency. That’s nearly 1 in 8. And for those on high doses for over a year, the risk jumps higher. The problem? Many patients feel fine. No symptoms. No warning. Then, during a cold, a car accident, or surgery, their body can’t ramp up cortisol-and they crash.What Is ACTH Stimulation Testing?
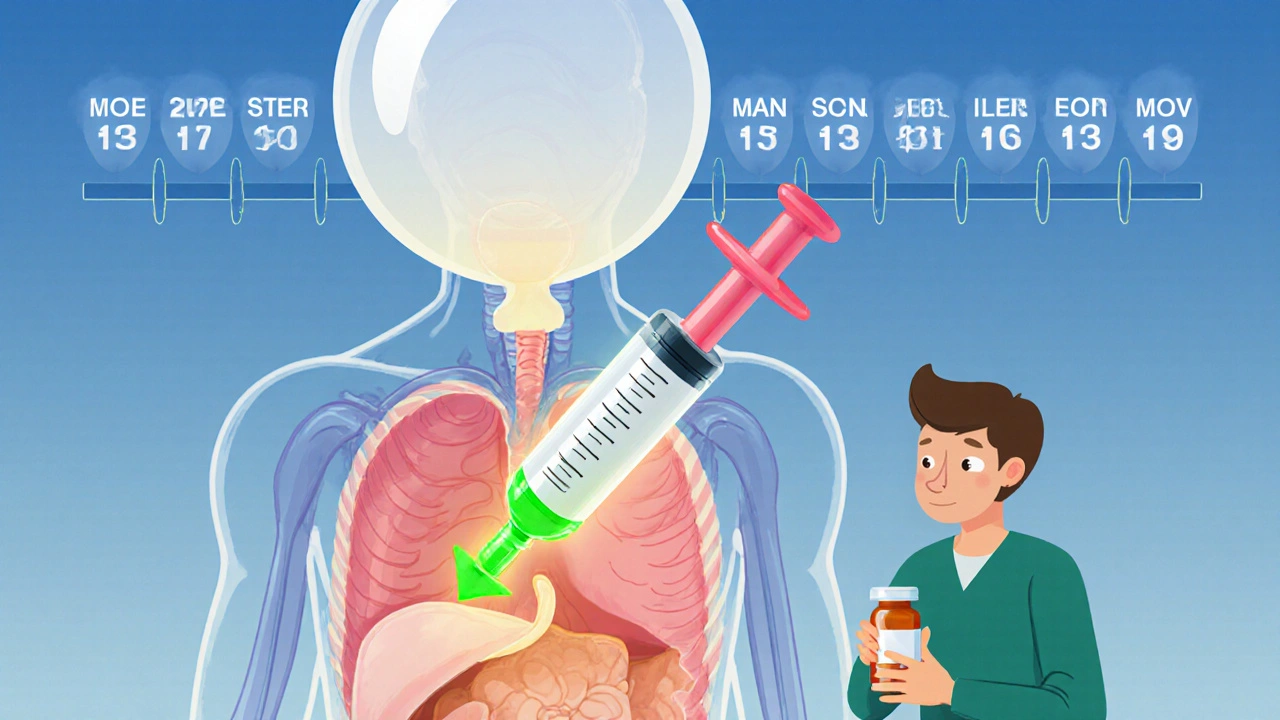
The ACTH stimulation test checks if your adrenals can still respond. It’s simple: you get a shot of synthetic ACTH (cosyntropin), usually 250 mcg, either into your muscle or vein. Then, blood is drawn before the shot and again at 30 and 60 minutes after. Your cortisol level tells the story. If your peak cortisol is 18-20 mcg/dL or higher, your adrenals are recovering. If it’s below 14 mcg/dL, you’re still suppressed. That means you need to keep tapering slowly-or stay on replacement doses longer. This isn’t just theory. A 2024 study from Mayo Clinic tracked 450 patients over five years. Those who followed ACTH-guided tapers had an adrenal crisis rate of just 1.2%. Those who didn’t test? It was 8.5%. That’s an 86% reduction in life-threatening events.When to Test-And When Not To
Timing matters. Testing too early gives false negatives. Your adrenals need time to wake up. The 2024 Endocrine Society guidelines say: test only after you’ve reached a physiologic dose-about 4-6 mg of prednisone per day. That’s the amount your body should naturally make. If you’ve been on steroids for less than 3-4 weeks, you likely don’t need testing. Your HPA axis usually recovers on its own. But if you’ve been on them for more than 3 months? Testing is recommended. Some experts, like Dr. Alessandro Prete, argue for routine testing at the 6-month mark for anyone on steroids longer than 6 months. It’s not just safer-it’s cost-effective. The tricky part? Not all doctors agree. The Endocrine Society says test only if you have symptoms or are high-risk. Others, like the Adrenal Insufficiency Coalition, say test everyone after 3 months. In practice, the most cautious approach wins: if you’ve been on steroids for over 12 months, test before stopping completely.
Tapering Schedules: One Size Doesn’t Fit All
There’s no universal taper. It depends on how long you’ve been on steroids and why. For 3-12 months of therapy, the PJ Nicholoff Protocol (used widely in neuromuscular diseases like Duchenne muscular dystrophy) recommends dropping prednisone by 2.5-5 mg every 1-2 weeks until you hit 10-15 mg/day. Then, reduce by 20-25% per week. At 5 mg/day, slow down even more-maybe 0.5-1 mg every 2-4 weeks. For over 12 months? Recovery takes longer. Experts say: one month of tapering for every month you were on steroids. So if you were on high-dose prednisone for 18 months, expect at least 18 months of slow tapering. Some need up to 2 years. Rushing this can lead to permanent adrenal damage. Replacement doses are precise: 4-6 mg prednisone daily, or 15-25 mg hydrocortisone split into three doses-10 mg in the morning, 5 mg at noon, 5 mg in the early afternoon. That mimics your body’s natural rhythm. Skipping the afternoon dose? You risk fatigue and low blood pressure by evening.What About Withdrawal Symptoms?
Many people confuse adrenal insufficiency with steroid withdrawal. They’re different. Withdrawal symptoms-fatigue, joint pain, nausea, anxiety, insomnia-are common in 35-45% of patients. They don’t mean your adrenals are failing. They mean your body is adjusting. The fix? Don’t panic. Don’t jump back to your old dose. Instead, pause the taper for 1-2 weeks at the last tolerated dose. Then try again, slower. True adrenal insufficiency? That’s when you feel worse even at replacement doses. You might have dizziness when standing, low blood sugar, or vomiting. That’s when you need a cortisol test-and likely to stay on replacement longer.
Real-World Challenges
The science is clear. The practice? Not so much. A 2022 study found that 68% of primary care doctors felt unprepared to manage ACTH testing. Why? Access. In rural areas, patients might drive three hours for a test. Wait times for endocrinology appointments can be 4-6 weeks. Some patients never get tested. Others skip follow-ups. That’s when emergencies happen. One ER doctor in Ohio told a Reddit thread: “I saw a 32-year-old collapse after stopping prednisone. She’d been on it for 14 months. Her PCP said, ‘Just cut it in half every week.’ She didn’t know what adrenal crisis was. She didn’t have a steroid card.” Patient advocacy groups report that 78% of people on long-term tapers feel anxious. 42% had severe withdrawal symptoms. The stress isn’t just physical-it’s emotional. You’re scared you’ll relapse. You’re scared you’ll crash. You’re scared you’ll be stuck on steroids forever.What You Can Do
If you’re tapering:- Get an ACTH test before stopping completely-if you’ve been on steroids for more than 3 months.
- Never skip your dose. Even if you feel fine, your body still needs cortisol.
- Carry a steroid alert card. It says you’re on or recently came off steroids. Emergency teams need to know.
- Know your stress dose rules. If you get sick, injured, or have surgery, you need 2-3x your normal dose. Don’t wait for symptoms.
- Track your symptoms. Write down fatigue, dizziness, nausea. Share it with your doctor. Don’t assume it’s “just stress.”
The Future Is Coming
New tools are on the horizon. The Endocrine Society is launching a mobile app in late 2024 to guide tapers and remind you when to test. The NIH is funding a point-of-care ACTH test-something you could get in your doctor’s office, not a lab. And Epic’s EHR system is adding HPA axis tracking modules in 2025. But the biggest change? Awareness. More doctors are learning. More patients are asking. More hospitals are requiring steroid cards and written taper plans before discharge. The message is simple: Long-term steroid use isn’t a quick fix. It’s a long recovery. And ACTH testing isn’t just a test-it’s a lifeline.How long does it take for adrenal glands to recover after stopping steroids?
Recovery time depends on how long you were on steroids. For therapy lasting 3-12 months, it can take 6-12 months. For over 12 months, experts recommend one month of tapering for every month of use-so 9 to 12 months or longer. Some patients need up to two years to fully recover cortisol production. ACTH stimulation testing helps determine when recovery is complete.
Can I stop steroids cold turkey after long-term use?
No. Stopping abruptly after long-term use can cause adrenal crisis-a medical emergency. Your body stops making cortisol, and your adrenals can’t restart on their own. Symptoms include low blood pressure, vomiting, confusion, and loss of consciousness. Always taper slowly under medical supervision with ACTH testing to monitor recovery.
What’s the difference between adrenal insufficiency and steroid withdrawal?
Adrenal insufficiency means your body can’t produce enough cortisol, confirmed by low cortisol levels on an ACTH test. Withdrawal symptoms-like fatigue, joint pain, or anxiety-are common during tapering but don’t mean your adrenals have failed. They’re your body adjusting. The key difference: withdrawal improves with rest and slow tapering; adrenal insufficiency requires continued steroid replacement until testing shows recovery.
Do I need an ACTH test if I’m on low-dose steroids?
If you’ve been on any dose of glucocorticoids for more than 3 months, yes. Even low doses can suppress your HPA axis. The 2024 Endocrine Society guidelines recommend testing before stopping, regardless of dose, if therapy lasted over 3-4 weeks. For doses below 5 mg prednisone daily, testing is especially important because symptoms may be subtle.
What should I do if I get sick during a steroid taper?
Increase your steroid dose immediately. During illness, injury, or surgery, your body needs 2-3 times your usual maintenance dose. For example, if you’re on 5 mg prednisone, take 10-15 mg until you recover. Never skip doses during stress. Always carry a steroid alert card and tell any medical provider you’re tapering off steroids.
Are there alternatives to ACTH stimulation testing?
Currently, no reliable alternative exists. Salivary cortisol tests are being studied but aren’t validated for this use. Morning serum cortisol levels alone aren’t enough-they don’t show adrenal reserve. ACTH stimulation remains the only test that measures your adrenal glands’ ability to respond under stress. Research is ongoing, but for now, it’s the gold standard.

angie leblanc
November 22, 2025 AT 23:09LaMaya Edmonds
November 24, 2025 AT 05:21See Lo
November 25, 2025 AT 21:10Chris Long
November 26, 2025 AT 10:39Liv Loverso
November 26, 2025 AT 13:36Steve Davis
November 28, 2025 AT 00:46Attila Abraham
November 28, 2025 AT 15:54Michelle Machisa
November 30, 2025 AT 01:40Ronald Thibodeau
November 30, 2025 AT 23:25Shawn Jason
December 1, 2025 AT 20:53Monika Wasylewska
December 3, 2025 AT 03:12Jackie Burton
December 3, 2025 AT 18:00Philip Crider
December 5, 2025 AT 08:36Diana Sabillon
December 5, 2025 AT 13:39neville grimshaw
December 7, 2025 AT 11:31Carl Gallagher
December 7, 2025 AT 19:29bert wallace
December 9, 2025 AT 02:24Neal Shaw
December 9, 2025 AT 23:54Hamza Asghar
December 10, 2025 AT 08:56