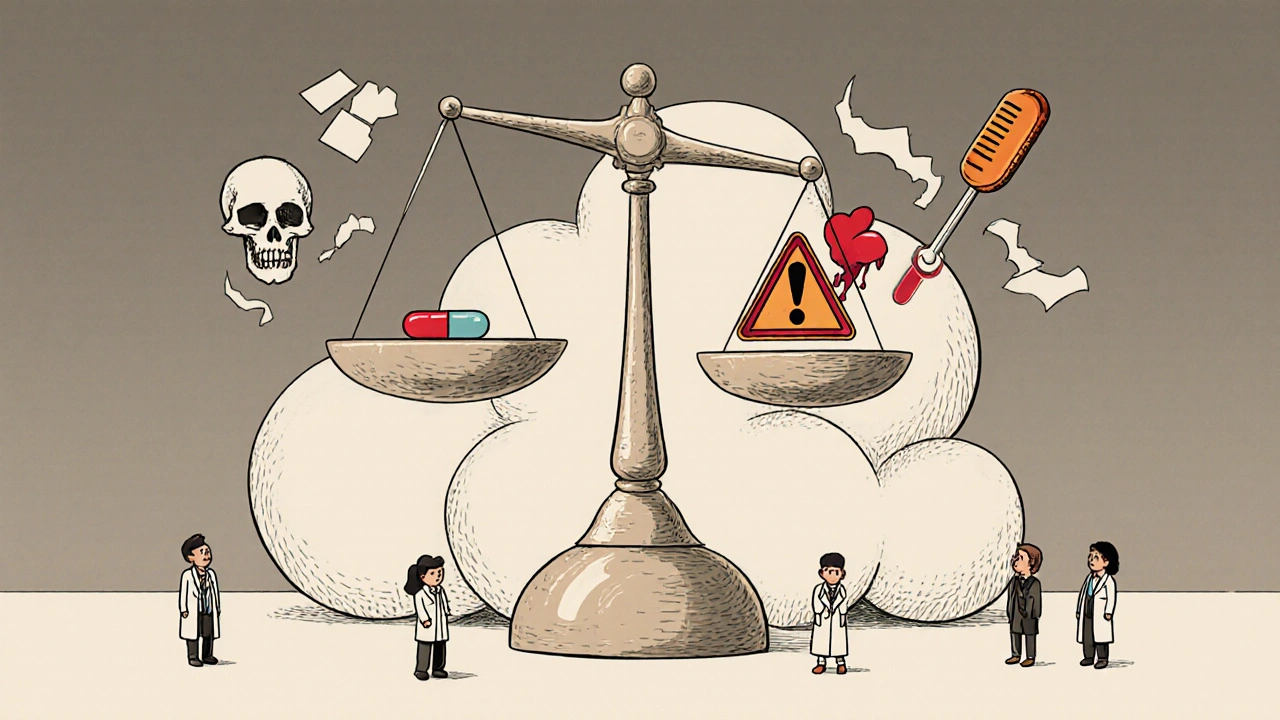
NTI drugs aren’t just another category of medication-they’re the ones where a tiny mistake can turn treatment into crisis. A 5% higher dose of warfarin might send your INR soaring into dangerous territory. A switch from one brand of levothyroxine to another could leave you fatigued, depressed, or worse. These aren’t hypothetical risks. They happen every day in clinics, hospitals, and homes across New Zealand and beyond. NTI stands for Narrow Therapeutic Index, meaning the gap between a helpful dose and a harmful one is razor-thin. One pill too many-or too few-and the consequences can be life-altering.
What Makes a Drug an NTI Drug?
Not all drugs are created equal when it comes to safety margins. Most medications have a wide buffer-you can miss a dose or take an extra one without major fallout. NTI drugs are different. Their therapeutic range is so narrow that even small changes in blood levels can cause treatment failure or serious toxicity. The U.S. FDA defines them as drugs where small differences in dose or blood concentration may lead to serious therapeutic failures or life-threatening side effects. That’s not a technical footnote-it’s a clinical red flag.
For example, digoxin, used for heart rhythm problems, has a therapeutic range of just 0.5 to 2.0 nanograms per milliliter. That’s less than a grain of salt dissolved in a liter of water. Go above 2.0, and you risk dangerous arrhythmias. Drop below 0.5, and the drug stops working. There’s no room for guesswork. The same applies to lithium, used for bipolar disorder. Its safe range is 0.6 to 1.2 mmol/L. A level of 1.5 can cause tremors, confusion, and kidney damage. At 2.0, it’s a medical emergency.
The Core NTI Drug List: What’s Actually on the Radar
There’s no single official global list of NTI drugs, but clinical practice and regulatory agencies agree on a core group. These are the medications that require the most careful handling:
- Warfarin - The classic NTI anticoagulant. Target INR is 2.0-3.0 for most conditions. A single INR above 4.0 increases major bleeding risk by over 7 times. Even small changes in diet, antibiotics, or supplements can throw it off balance.
- Digoxin - Used for heart failure and atrial fibrillation. The window between effective and toxic is less than 1.5 ng/mL. Toxicity can cause nausea, visual disturbances, and fatal heart rhythms.
- Lithium - The go-to mood stabilizer. Monitoring every 3-6 months isn’t optional-it’s mandatory. Levels above 1.5 mmol/L require immediate action.
- Phenytoin - An older but still widely used antiepileptic. Therapeutic range: 10-20 mcg/mL. Too low? Seizures return. Too high? Nystagmus, slurred speech, even coma.
- Tacrolimus and Cyclosporine - Lifesaving immunosuppressants for transplant patients. Tacrolimus trough levels must stay between 5-15 ng/mL. A level of 20 ng/mL can cause kidney failure. These are monitored weekly in the early post-transplant phase.
- Carbamazepine - Another antiepileptic and mood stabilizer. Therapeutic range: 4-12 mcg/mL. It interacts with dozens of other drugs, making dose adjustments tricky.
- Levothyroxine - The most common thyroid replacement. Sounds harmless, right? Wrong. Even small changes in formulation or absorption can shift TSH from 1.2 to 8.7 mIU/L, as documented in real patient cases. That’s the difference between feeling normal and being severely hypothyroid.
- Valproic Acid - Used for epilepsy and bipolar disorder. Therapeutic range: 50-100 mcg/mL. Liver toxicity and pancreatitis are real risks at higher levels.
Some newer drugs are joining this list. Cancer therapies like axitinib, ponatinib, and olaparib are now classified as NTI because their effectiveness and toxicity are tightly linked to precise blood concentrations. These aren’t just experimental-they’re standard care for certain cancers today.
Why Generic Substitutions Can Be Dangerous
One of the biggest risks with NTI drugs isn’t the dose-it’s the switch. Many patients are unaware that switching from brand-name to generic-or even between two different generic manufacturers-can cause significant changes in blood levels. This isn’t speculation. In 2023, a Reddit post from a pharmacist detailed a case where a 62-year-old woman’s TSH jumped from 1.2 to 8.7 after her pharmacy switched her levothyroxine brand. It took three months and five dose adjustments to stabilize her. That’s not an outlier-it’s a common story.
The FDA requires stricter bioequivalence standards for NTI drugs. For regular drugs, generics must match the brand within 80-125% of the original. For NTI drugs, that range tightens to 90-111%. But even within that tighter range, small differences in absorption, fillers, or coating can matter. That’s why 47 U.S. states have laws restricting automatic substitution of NTI drugs without a doctor’s explicit permission. In New Zealand, MEDSAFE advises that NTI drugs like warfarin, cyclosporine, and anticonvulsants should not be considered interchangeable without physician authorization.

Monitoring Isn’t Optional-It’s the Standard of Care
There’s no way around it: if you’re on an NTI drug, regular blood tests aren’t a suggestion-they’re a requirement. Here’s what’s typically needed:
- Warfarin: INR checked every 3-5 days after starting, then weekly until stable, then every 4-6 weeks.
- Lithium: Serum levels every 3-6 months, more often after dose changes or if symptoms appear.
- Digoxin: Level checked after 5-7 days of starting or changing dose, then every 6-12 months if stable.
- Tacrolimus: Trough levels checked 3 times a week in the first month after transplant, then weekly, then monthly.
- Phenytoin: Trough levels checked after 7-10 days of dose change, then every 3-6 months.
These tests aren’t just paperwork. They prevent hospitalizations. A 2022 survey found that 87% of hospital pharmacists consider therapeutic drug monitoring essential for NTI drugs. And 73% say they’ve personally stopped a dosing error in the past year.
What Happens When Monitoring Fails
Missed appointments, forgotten blood tests, or ignored symptoms can lead to disaster. A 2022 study in JAMA Internal Medicine found that 32% of lithium patients miss their monitoring appointments. That’s over one in three people taking a drug that can kill them if not watched closely.
And it’s not just about forgetting. Electronic health records still lag behind. Only 45% of hospital systems have automated alerts when NTI drug levels go out of range. That means someone has to manually check-and sometimes, they don’t.
The cost is another barrier. A single blood test for an NTI drug can cost $25-$150. While Medicare and some private insurers cover 80%, patients still pay out-of-pocket. For those on fixed incomes, that’s a real deterrent.
What You Can Do: A Practical Guide
If you’re prescribed an NTI drug, here’s what you need to do:
- Know your drug. Ask your doctor or pharmacist: Is this an NTI drug? What’s my target level?
- Keep a log. Write down your dose, when you take it, and any side effects. Note any new medications, supplements, or dietary changes.
- Never switch brands without talking to your doctor. Even if the pharmacy says it’s "the same," ask if it’s interchangeable.
- Attend every blood test. Don’t skip it because you "feel fine." Levels can change without symptoms.
- Carry a card. Keep a small note in your wallet or phone that lists your NTI drug, dose, and target level. In an emergency, that could save your life.
There’s no magic fix. NTI drugs require vigilance. But with the right awareness and habits, they can be managed safely for years-even decades.
Where the Field Is Headed
The future of NTI drug management is getting smarter. The NIH is funding a $15 million study to use genetic testing to predict how people metabolize warfarin and phenytoin. Early results show a 40% faster time to stable dosing. AI tools are being tested in hospitals to predict when a patient’s level might drift based on diet, medications, and even weather patterns.
Wearable biosensors that measure drug levels in sweat or interstitial fluid are in early development. Imagine a patch that tells you your tacrolimus level without a needle. That’s not science fiction-it’s coming within the next five years.
But until then, the rules haven’t changed: know your drug, test regularly, and never assume generics are interchangeable. Your life depends on it.
Are all blood thinners NTI drugs?
No. Warfarin is an NTI drug because its therapeutic window is very narrow and requires frequent INR monitoring. Newer blood thinners like apixaban, rivaroxaban, and dabigatran have wider therapeutic windows and don’t require routine blood testing. However, some experts still consider them to have a "narrow therapeutic range" due to bleeding risks, especially in elderly or kidney-impaired patients. Regulatory bodies like the FDA are reviewing whether to classify these newer agents as NTI drugs in future guidance.
Can I switch from brand to generic NTI drugs?
It’s not recommended without your doctor’s approval. Even though generics must meet strict bioequivalence standards for NTI drugs, small differences in formulation can still cause blood levels to shift. Cases have been documented where switching levothyroxine brands caused TSH levels to jump from normal to severely high, requiring months to correct. Always consult your prescriber before any switch.
Why is lithium so tightly monitored?
Lithium has a very narrow margin between therapeutic and toxic levels. The safe range is only 0.6-1.2 mmol/L. At 1.5 mmol/L, you may experience tremors, confusion, or nausea. At 2.0 mmol/L or higher, it can cause seizures, kidney damage, or coma. Lithium is also eliminated by the kidneys, so dehydration, salt intake, or kidney changes can quickly raise levels. Regular monitoring prevents these life-threatening outcomes.
Do NTI drugs interact with other medications?
Yes, and that’s one of the biggest risks. Many NTI drugs are metabolized by the same liver enzymes. For example, phenytoin and carbamazepine interact with dozens of antibiotics, antifungals, and even grapefruit juice. Warfarin interacts with common painkillers like ibuprofen and supplements like vitamin K. Always tell your doctor and pharmacist about every medication, herb, or supplement you take-even over-the-counter ones.
Is there a cure or alternative to NTI drugs?
There’s no cure for the conditions NTI drugs treat-like epilepsy, bipolar disorder, or organ transplant rejection. But newer treatments are emerging. For example, some patients with atrial fibrillation can now use non-NTI anticoagulants instead of warfarin. For epilepsy, newer antiseizure drugs may have wider safety margins. However, for many, NTI drugs remain the most effective option. The goal isn’t to eliminate them-it’s to use them safely through strict monitoring and patient education.
Final Thought: Safety Is a Habit, Not a One-Time Event
NTI drugs demand more than a prescription. They demand attention. They require you to be your own advocate-tracking doses, asking questions, showing up for blood tests, and refusing substitutions without approval. It’s not always convenient. It’s not always cheap. But for the people who rely on these medications, it’s the only thing standing between stability and catastrophe.

David Barry
November 13, 2025 AT 07:48Let’s be real-NTI drugs aren’t just risky, they’re a fucking administrative nightmare. Pharmacies swap generics like trading cards, doctors don’t bother updating charts, and patients? They think ‘same pill, same effect.’ Wrong. One study showed 38% of patients on levothyroxine had TSH shifts after a brand switch-no warning, no consent. This isn’t pharmacology, it’s Russian roulette with a thyroid.
Benjamin Stöffler
November 14, 2025 AT 10:35Here’s the thing: the FDA’s 90–111% bioequivalence buffer for NTI drugs? It’s a mathematical illusion. Bioavailability isn’t linear-it’s chaotic, context-dependent, and utterly dependent on gut flora, meal timing, and whether you drank coffee 20 minutes before ingestion. The system assumes homogeneity. Humans? We’re messy. So yes, the numbers look tight… but biology doesn’t care about your spreadsheets.
And don’t get me started on the ‘generic is cheaper’ mantra-it’s a neoliberal fantasy. You save $3 on a pill, then spend $12,000 on an ER visit because your lithium spiked. Who’s really paying?
Also: why is warfarin still the gold standard? It’s a 1950s anticoagulant with 200+ drug interactions. We’ve got DOACs that don’t require INR checks, yet we cling to this relic because ‘it’s cheaper.’ That’s not clinical wisdom-it’s institutional inertia dressed up as tradition.
And let’s not pretend monitoring is ‘standard care.’ In rural clinics, patients drive 90 miles for a blood draw. That’s not compliance-it’s a miracle. We treat NTI drugs like they’re in a lab, but real people live in the real world-with jobs, childcare, and no transportation.
Meanwhile, AI tools predicting drift based on weather? Cute. But if your patient can’t afford the test, does it matter? Technology without equity is just another form of exclusion.
And yes, I’ve seen patients on tacrolimus who lost their kidneys because their pharmacy switched brands and no one told them. No malice. Just systemic negligence. That’s the real NTI drug: bureaucracy.
The future isn’t wearables or genetic testing. It’s universal healthcare with pharmacist-led monitoring. Until then, we’re just rearranging deck chairs on the Titanic.
And don’t even get me started on vitamin K supplements. One capsule, and your INR plummets. Patients don’t know this. Their ‘natural remedy’ is a chemical grenade.
So yes-know your drug. But also demand better systems. Because vigilance shouldn’t be the patient’s job.
It’s the system’s responsibility.
Alex Ramos
November 16, 2025 AT 00:14This is such an important post-thank you!! I’m a pharmacy tech and I see this daily. One lady came in crying because her TSH went from 2.1 to 11.2 after her generic levothyroxine switched brands. She thought she was ‘just fine’ until she couldn’t get out of bed. We called her doctor immediately. She’s on the same brand now, and she’s back to normal.
Always check the label-even if it’s the same name, the manufacturer changes. And yes, carry that card!! I keep one in my wallet too.
Also-don’t skip bloodwork because you ‘feel fine.’ I’ve seen people with lithium levels at 1.8 and zero symptoms. By the time they feel bad? It’s too late. Stay vigilant!! 💪
edgar popa
November 17, 2025 AT 11:11Just had my INR checked last week-4.2. Scared the crap outta me. Turns out I started taking turmeric for my knees. Never knew it thinned blood. Lesson learned. Always tell your doc about every pill, powder, or tea. Seriously.
Eve Miller
November 18, 2025 AT 14:57It’s appalling that 47 U.S. states have laws restricting NTI generic substitutions, yet 3 states still allow it without physician consent. This isn’t a ‘debate’-it’s a public health failure. The FDA’s guidelines are clear. The science is clear. The deaths are documented. And yet, some pharmacies still prioritize profit over safety. Shameful.
Patients are not lab rats. They are not interchangeable variables. They are people. And their lives depend on consistency-not corporate convenience.
Amie Wilde
November 19, 2025 AT 00:10My mom’s on lithium. She’s 72. We do her bloodwork every 3 months like clockwork. She hates it. But I make her go. One time she skipped it ‘cause she felt ‘fine.’ Next week she was dizzy, confused, and almost got taken to the hospital. Now she carries her test dates on her phone calendar. No more ‘fine.’ Just facts.
Chrisna Bronkhorst
November 20, 2025 AT 01:38NTI drugs are the reason I stopped trusting pharmacies. My cousin switched from brand to generic tacrolimus after transplant. His levels dropped. Rejection started. Took 3 months to fix. He lost 40 pounds. Now he pays $200 extra monthly for the brand. And he’s lucky-he had insurance. What about the guy in rural Alabama with no car? He’s dead before the system notices.
It’s not about the drug. It’s about the system. And the system is broken.
Esperanza Decor
November 21, 2025 AT 05:12Okay I just read this whole thing and I’m shaking. I didn’t know any of this. I’m on carbamazepine and I thought generics were the same. I just switched last month. I’ve been foggy and nauseous. I thought it was stress. Now I’m calling my doctor tomorrow. Thank you for this. Seriously. This could’ve killed me.
Also-why isn’t this taught in high school? Like, this should be in health class. Not just ‘take your pills.’ But ‘here’s how one pill can kill you if you don’t watch it.’
And yes, I’m writing this on my phone right now and I’m gonna screenshot the list. I’m not taking chances anymore.
Mark Rutkowski
November 21, 2025 AT 19:46There’s a quiet dignity in the way NTI drugs force us to become guardians of our own biology. We’re not just patients-we’re scientists, record-keepers, advocates, and sometimes, detectives. We track our meals, our sleep, our stress, our supplements-all to keep a single molecule within a sliver of safety. It’s exhausting. It’s lonely. But it’s also profoundly human.
These drugs don’t just treat illness-they demand awareness. They turn routine into ritual. And in a world that rewards speed, distraction, and disposability, that’s revolutionary.
So yes, the system fails. Yes, the costs are unfair. But the act of showing up-for the blood draw, for the refill, for the conversation with your pharmacist-that’s where healing begins. Not in the lab. Not in the algorithm. In the quiet, stubborn choice to care.
And that? That’s worth more than any pill.
Deepa Lakshminarasimhan
November 22, 2025 AT 10:45Wait… so you’re telling me this whole NTI thing is real? Like… the government’s hiding this? Why? So they can sell more tests? More brand-name drugs? I’ve been reading about how the FDA and pharma companies are linked. Maybe they want us dependent on constant monitoring so they keep making money off our fear. I don’t trust any of this anymore.
What if the ‘narrow window’ is just a scam to keep us buying blood tests and brand pills? I’m switching to herbal remedies. No more pharmaceuticals. I’m done.
Ryan Everhart
November 24, 2025 AT 08:06So… you’re saying if I take my lithium with a big salad instead of a burger, my levels might drop? And if I get a cold and my kidneys slow down, I could overdose? And if my pharmacy switches my brand, I might not know until I’m hallucinating?
Wow. So… I’m basically a walking chemistry experiment.
Thanks for the clarity.
Gary Hattis
November 25, 2025 AT 16:37I’m from South Africa-we don’t have the same access to monitoring as the U.S. But we still use these drugs. I’ve seen patients on cyclosporine who get their levels checked… once a year. If they’re lucky. Some take their meds with tea, some with milk, some skip meals. They don’t know it matters. No one told them.
This post? It’s not just for Americans. It’s for every person in every country who’s been told, ‘Just take it.’
Education saves lives. Not just prescriptions.
Alyssa Lopez
November 27, 2025 AT 14:24Y’all are overreacting. NTI drugs? Pfft. I’ve been on warfarin for 10 years. I take my pill, I eat my greens, I get my INR. Done. If you can’t handle it, don’t take it. Stop whining about generics. America’s so soft. In my day, we took what we got and didn’t cry about it. This is why our healthcare’s so expensive-because everyone’s scared of a pill.
Also, I think the FDA is just trying to control us. You think they really care? They just want to sell more tests. Wake up.
Alex Ramos
November 28, 2025 AT 11:08Just wanted to reply to @AlyssaLopez-your attitude is exactly why people die. You’re not ‘tough’-you’re reckless. People aren’t ‘whining.’ They’re surviving. And if you think generics are ‘the same,’ you’ve never watched someone go into lithium toxicity. I’ve seen it. It’s not a ‘soft’ thing. It’s a medical emergency.
Stop minimizing. Start listening.