Topical Steroid Risk Assessment Tool
This tool helps you understand your risk of developing skin atrophy or withdrawal symptoms from topical steroid use. Answer the questions below to get personalized risk assessment and recommendations.
Your Risk Assessment
When you have eczema, psoriasis, or a stubborn rash, a topical corticosteroid cream can feel like a miracle. It calms the redness, stops the itching, and gives you back control of your skin. But what happens when that miracle starts to backfire? Over time, especially with strong steroids used too long or on sensitive areas, your skin can begin to break down-not just in appearance, but in function. This isn’t rare. It’s documented, predictable, and often preventable.
How Topical Steroids Thin Your Skin
Topical corticosteroids work by suppressing inflammation. That’s their job. But they don’t just turn off inflammation-they also slow down the natural repair systems in your skin. Keratinocytes, the cells that make up the outer layer, stop multiplying as fast. Fibroblasts, the cells that build collagen and elastin, get the signal to cut back on production. Within days, even with potent steroids, the structure of your skin starts to change.The epidermis thins. The dermis loses its support network of collagen. Ceramides, cholesterol, and fatty acids-the lipids that hold your skin barrier together-drop by as much as 50% in some cases. This isn’t just surface-level dryness. It’s a structural collapse. Your skin becomes more fragile, more transparent, and less able to hold onto moisture. That’s why you might notice fine lines that look like wrinkles, even if you’re young. Dermatologists call these "elephant wrinkles"-deep, persistent creases that don’t fade with moisturizer.
Even more concerning? The damage isn’t always visible right away. You might not see thinning until months after you’ve been using the cream. But the biochemical changes start within 72 hours. Studies show that the stratum corneum-the outermost protective layer-takes longer to recover than you’d expect. Once collagen fibers are permanently broken down, they don’t regenerate. That’s when striae (stretch marks) form. And once they’re there, they’re permanent.
Why Some Areas Are More at Risk
Not all skin is created equal. The skin on your face, eyelids, armpits, groin, and inner thighs is naturally thinner. That makes it more vulnerable. Applying a Class I or II corticosteroid (the strongest types) to your face for just two weeks can trigger atrophy in up to 17% of users, according to a 2021 analysis of over 8,000 patients.Children are even more sensitive. Their skin is thinner and absorbs more. A parent using a potent steroid on a baby’s diaper rash for more than a few days risks causing lasting damage. The same goes for elderly patients-whose skin is already losing collagen naturally. And sun exposure makes it worse. UV rays break down collagen too. When you combine steroid-induced suppression with sun damage, the effect is cumulative. One study showed unprotected skin in atrophic areas lost 42% more collagen than protected skin over the same period.
When Thinning Leads to Infection
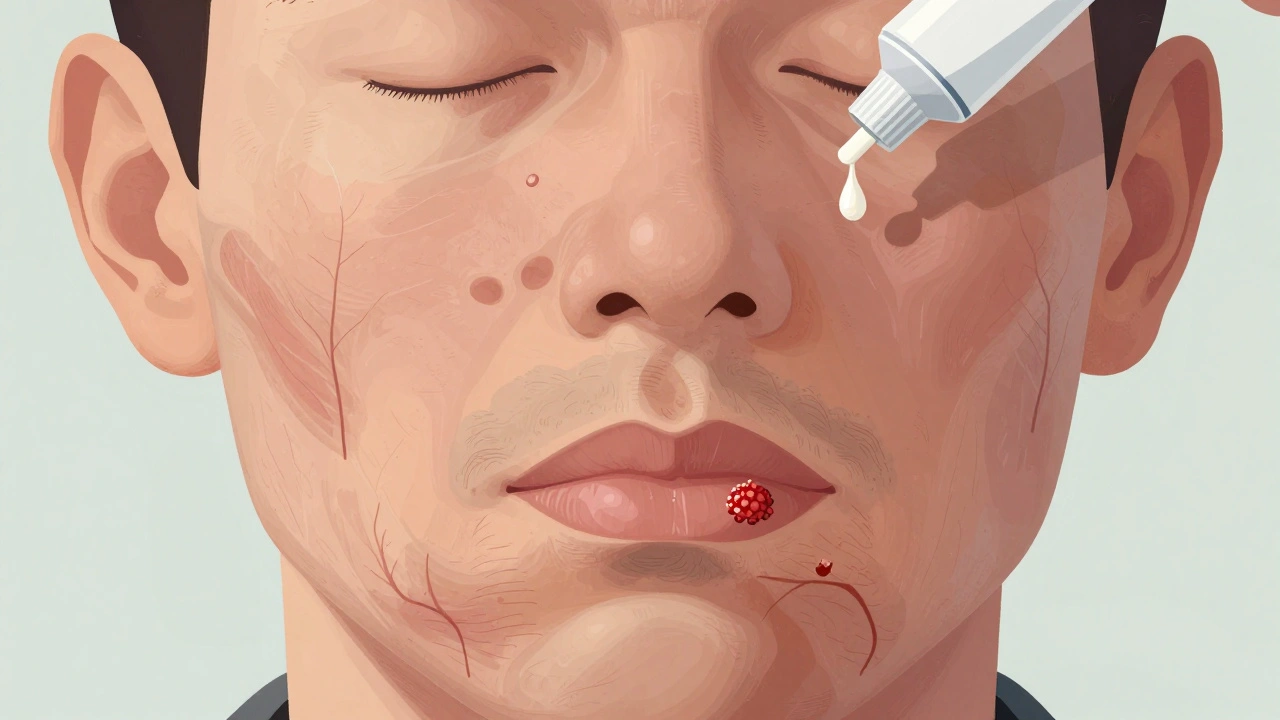
A weakened skin barrier doesn’t just mean dryness and wrinkles. It means your skin can’t defend itself. Bacteria, fungi, and viruses slip through more easily. The most common infections linked to long-term steroid use are:- Fungal infections: Candida albicans thrives in warm, moist areas like the groin or under the breasts. Steroids suppress the immune response locally, letting yeast overgrow. You’ll see red, scaly patches with raised edges-often mistaken for eczema flare-ups.
- Bacterial infections: Staphylococcus aureus, the same bacteria that causes impetigo, takes advantage of broken skin. You might get pus-filled bumps, crusting, or oozing that doesn’t improve with moisturizer.
- Viral infections: Herpes simplex can spread rapidly under steroid cover. What looks like a bad eczema flare could be a herpes outbreak. These lesions are painful, blistering, and need antiviral treatment, not more steroid cream.
Perioral dermatitis is another classic sign. It shows up as small red bumps around the mouth, nose, or eyes. People often think it’s acne and reach for stronger steroids. That only makes it worse. The condition can persist for months after stopping the steroid, and it’s notoriously hard to treat without a proper diagnosis.

The Withdrawal Trap
Many people stop using steroids cold turkey when they notice damage. That’s when things get worse. The skin, now dependent on the anti-inflammatory effect, goes into overdrive. Inflammation rebounds harder than before. This is called Topical Steroid Withdrawal (TSW).The pattern is consistent: Within a week of stopping, you get burning, stinging, and bright red skin. It might feel like a sunburn that won’t go away. After two weeks, peeling starts. Then another flare hits-sometimes worse than the first. Each flare gets shorter, but the recovery periods get longer. In one study of 127 patients, the average withdrawal phase lasted 6-12 months. Reddit communities with thousands of members report average recovery times of 8.2 months, with some taking over two years.
What makes TSW so hard to manage? Doctors often don’t recognize it. Patients are told it’s "just eczema returning" or "allergic reaction." They’re prescribed more steroids, creating a cycle that’s nearly impossible to break. The burning sensation can be so severe that people can’t wear makeup, sleep through the night, or leave the house.
How to Use Steroids Safely
You don’t have to avoid topical corticosteroids. You just need to use them like a tool-not a crutch.- Use the weakest strength that works. Start with Class V or VI. Only move up if absolutely necessary.
- Limit duration. No more than 2-4 weeks on the face or sensitive areas. For body areas, 4-6 weeks max.
- Apply only to active flare-ups. Don’t use daily as maintenance unless directed by a dermatologist.
- Avoid occlusion. Don’t wrap skin in plastic or tight clothing after applying steroid cream-it increases absorption and risk.
- Never use on broken or infected skin. If it’s oozing, crusting, or painful, see a doctor. You might need antibiotics or antifungals first.
For long-term control, consider steroid-sparing options. Calcineurin inhibitors like tacrolimus or pimecrolimus are FDA-approved for eczema and don’t cause atrophy. Newer agents like crisaborole and dual-soft glucocorticoid agonists (currently in trials) show promise in reducing inflammation without suppressing collagen.

Repairing the Damage
If you’ve already developed atrophy or are in withdrawal, stopping the steroid is step one. But you need to rebuild.Barrier repair creams with ceramides, cholesterol, and free fatty acids in a 3:1:1 ratio are the gold standard. A 2020 clinical trial found these creams improved skin barrier function by 68.4% in eight weeks. Look for products labeled "ceramide-dominant" or "skin-identical lipids." Avoid fragrances, alcohol, and harsh exfoliants.
Sun protection isn’t optional. Use SPF 50+ daily, even indoors. UVA rays penetrate windows and accelerate collagen loss in damaged skin. Mineral sunscreens with zinc oxide are less irritating.
Patience is your best ally. Recovery isn’t linear. Some days will feel better. Others will feel worse. But with time and proper care, most people see improvement. The skin doesn’t return to its original thickness, but it regains function, resilience, and comfort.
What’s Changing in the Medical World
Regulators are catching up. The FDA required atrophy warnings on all topical steroid packaging since 2010. The EMA followed in 2015. In 2022, the UK’s MHRA issued specific guidelines for pharmacists and doctors to educate patients on risks.Meanwhile, research is moving fast. The NIH is testing a new topical formula that combines low-dose corticosteroids with fibroblast growth factor. Early results show a 63% drop in atrophy compared to standard treatment. The global market for steroid-sparing therapies is projected to grow from $1.2 billion in 2023 to $3.8 billion by 2028.
Topical corticosteroids aren’t going away. They’re too effective for too many conditions. But the era of long-term, unsupervised use is ending. The future is targeted, short-term, and paired with barrier repair and monitoring.
Can skin atrophy from steroids be reversed?
Mild atrophy can improve over months after stopping steroids, especially with barrier repair creams and sun protection. But once striae (stretch marks) form or collagen is permanently lost, the damage is irreversible. The skin can regain function and thickness to some degree, but it won’t look or feel exactly like it did before.
How long does topical steroid withdrawal last?
Withdrawal varies by individual and duration of steroid use. For most, flares last 6-12 months. People who used potent steroids for over a year often experience symptoms for 18-24 months. Recovery isn’t linear-there are good days and bad days. The key is consistency with barrier repair and avoiding triggers like heat, sweat, and harsh skincare.
Are over-the-counter steroid creams safe?
Even low-potency OTC hydrocortisone (1%) can cause atrophy if used daily for more than two weeks. Many people use these creams for months without realizing the risk. The label says "for up to 7 days," but people ignore that. If you’ve been using it longer, stop and switch to a ceramide moisturizer. Don’t assume "weaker" means "safe for long-term use."
What should I use instead of steroid creams?
For eczema and similar conditions, calcineurin inhibitors like tacrolimus or pimecrolimus are first-line alternatives. Crisaborole is another non-steroid option. For mild cases, high-quality barrier repair moisturizers with ceramides, cholesterol, and fatty acids can manage symptoms long-term. Always consult a dermatologist before switching-some conditions need medical supervision.
Is steroid-induced skin thinning common?
Yes. In long-term users, skin atrophy occurs in about 17% of cases. Striae affect 7.2%, and perioral dermatitis appears in 4.3%. These numbers rise significantly with stronger steroids, larger application areas, and use on the face or in children. It’s not rare-it’s underreported because many patients don’t connect their skin changes to the cream they’ve been using.
If you’ve been using a topical steroid for more than a few weeks and notice thinning, redness that won’t fade, or persistent burning after stopping, don’t wait. See a dermatologist. The sooner you stop the cycle, the sooner your skin can heal.

Sangram Lavte
December 8, 2025 AT 10:19Topical steroids are a double-edged sword. I’ve seen patients go from clear skin to paper-thin with striae in under 6 months. The docs don’t warn you enough. It’s not just eczema-it’s a slow-motion skin collapse.
Nicholas Heer
December 9, 2025 AT 03:14THIS IS A BIG PHARMA COVERUP. THEY KNOW STEROIDS DESTROY YOUR SKIN BUT THEY KEEP SELLING IT BECAUSE YOU’LL COME BACK FOR MORE. THE FDA? IN BED WITH BIG DERM. THEY’RE SELLING YOU A SLOW DEATH IN A TUBE. #STEROIDCONSPIRACY
Stacy here
December 10, 2025 AT 20:18Listen-I’ve been there. Burned out my face with hydrocortisone for 18 months. Thought it was acne. Turned out to be perioral dermatitis on steroids. I cried every night. But I switched to ceramide creams, stopped everything cold, and after 10 months? My skin’s alive again. It’s not perfect, but I can wear makeup. I can sleep. You can do this. It’s hell, but it’s worth it.
Wesley Phillips
December 12, 2025 AT 14:18Actually the collagen loss isn’t entirely irreversible-there’s emerging data on fibroblast reactivation via low-level laser therapy. Most people don’t know this because dermatology’s still stuck in the 90s. You’re not just a patient-you’re a data point in a flawed paradigm.
Olivia Hand
December 13, 2025 AT 03:26I used OTC hydrocortisone for my eyelids because I thought ‘it’s just 1%’. Two months later, my skin looked like tissue paper. I didn’t cry-I just stared. That’s when I realized: I’d been poisoning myself with something I thought was harmless. Now I use only barrier creams. No more quick fixes.
Desmond Khoo
December 14, 2025 AT 19:08Bro this hit different 😭 I used steroid cream on my arms for 3 years thinking it was helping. Now I have stretch marks that look like spiderwebs. I started ceramide lotion 6 months ago and my skin’s finally breathing again. You’re not alone. Healing is slow but real. 💪✨
Jane Quitain
December 15, 2025 AT 20:04i just found out my mom used steroid cream on my baby brother for his rash for 6 months… i think he’s gonna have scars forever. why do parents not know this???
Ted Rosenwasser
December 17, 2025 AT 04:40Let’s be real-TSW isn’t even a real diagnosis. It’s just rebound inflammation from immunosuppression. The Reddit community is hyping it up like it’s a cult. You stop steroids, your skin reacts. Shocking. Next you’ll say coffee causes adrenal fatigue.
Ashley Farmer
December 18, 2025 AT 10:52To anyone reading this and feeling hopeless-please know you’re not broken. Your skin isn’t failing you. It’s been betrayed by something meant to help. Healing takes time, but you’re not alone. I’ve walked this path. You’ll find your rhythm again.
David Brooks
December 18, 2025 AT 11:05STOP USING STEROIDS. NOW. I DID. I REGRET NOTHING. MY SKIN IS STILL WEIRD BUT IT’S MINE AGAIN. YOU GOT THIS. 💪🔥
Kurt Russell
December 19, 2025 AT 22:34Just read this and cried. I’m 32 and my face looks like an 80-year-old’s. I thought I was aging. Turns out, it was the cream I used for my acne. I’ve been off for 14 months. My skin’s not back to normal-but I can feel the difference. It’s breathing. I’m breathing. This post? Lifesaver.