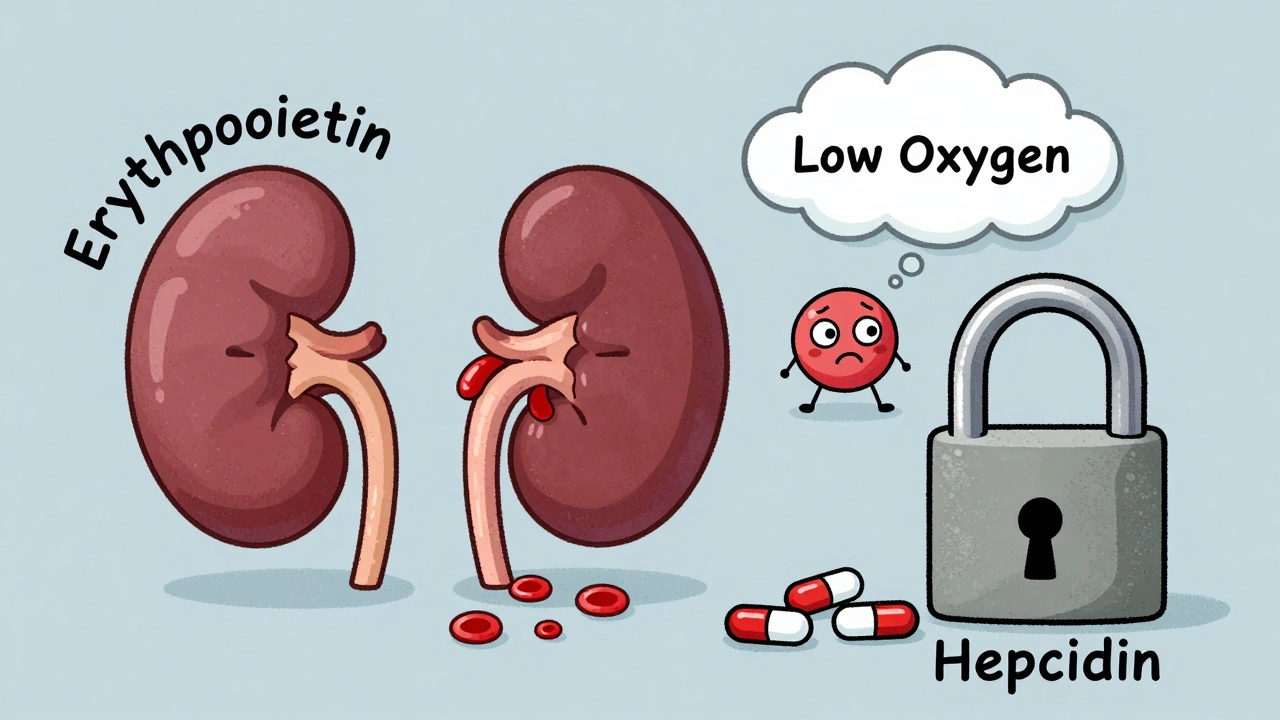
When your kidneys start to fail, they don’t just stop filtering waste-they also stop making a hormone your body needs to make red blood cells. That hormone is erythropoietin. Without it, your red blood cell count drops, leaving you tired, short of breath, and pale. This isn’t just normal fatigue. It’s anemia caused by chronic kidney disease (CKD), and it affects nearly 90% of people on dialysis and over half of those with advanced CKD not yet on dialysis.
Why Kidneys Fail to Make Red Blood Cells
Your kidneys produce erythropoietin in response to low oxygen levels in the blood. When kidney function declines-due to diabetes, high blood pressure, or other causes-this signal gets lost. The result? Your bone marrow doesn’t get the message to make more red blood cells. The anemia that follows is called normocytic and normochromic, meaning your red blood cells are the right size and color, but there just aren’t enough of them.
But it’s not just a lack of erythropoietin. In CKD, inflammation and iron problems make things worse. Your body holds onto iron like it’s gold, even when you’re low. This is thanks to a hormone called hepcidin, which spikes during kidney disease and blocks iron from moving into your bloodstream. So even if you eat iron-rich foods or take pills, your body can’t use it. That’s why oral iron often fails in CKD patients.
Iron Therapy: The First Step, Not the Last
Before you even think about erythropoietin injections, you need to fix your iron. The 2025 KDIGO guidelines (the most current international standard) say this clearly: if your ferritin is below 100 mcg/L, you have absolute iron deficiency-and you need IV iron right away. Even if your ferritin is between 100 and 500 mcg/L, but your transferrin saturation (TSAT) is under 20-30%, you still have functional iron deficiency. That means your body has iron stored, but it’s locked up and unusable.
Oral iron? It’s mostly useless here. Studies show only 30-40% of oral iron gets absorbed in CKD patients because of hepcidin. Meanwhile, IV iron-like iron sucrose or ferric carboxymaltose-bypasses the gut entirely. A single 400 mg dose can boost hemoglobin by nearly 1.5 g/dL in just four weeks. That’s why IV iron is now standard for everyone on hemodialysis. In 2010, only 48% of dialysis patients got IV iron. By 2022, that number jumped to 87%.
Patients often complain about a metallic taste or flu-like symptoms after the infusion, but these are usually mild and short-lived. The real danger? Giving too much. If ferritin climbs above 800 mcg/L, you risk iron overload, which can damage your heart and liver. That’s why doctors monitor levels monthly and stop IV iron when ferritin hits 700-800 mcg/L and TSAT goes above 40%.
Erythropoietin Therapy: What It Is and How It Works
Once iron levels are in range, and hemoglobin is still below 10 g/dL, doctors add an erythropoiesis-stimulating agent (ESA). These are synthetic versions of erythropoietin. The most common ones are epoetin alfa, epoetin beta, and darbepoetin alfa. There’s also Retacrit, a biosimilar that works just like epoetin alfa but costs less.
For patients not on dialysis, ESAs are usually given under the skin. For those on hemodialysis, they’re given straight into the bloodstream during treatment. A typical starting dose for darbepoetin alfa is 0.45 mcg/kg once a week. Most patients see their hemoglobin rise by 1-2 g/dL within 2-6 weeks.
But here’s the catch: ESAs aren’t magic. They can be dangerous if used wrong. The TREAT trial in 2009 showed that pushing hemoglobin above 13 g/dL increased stroke risk by 32%. That’s why the 2025 KDIGO guidelines say: keep hemoglobin between 10 and 11.5 g/dL. Not 12. Not 13. 10-11.5. This range reduces the need for blood transfusions, improves energy, and lowers heart risks-without increasing clots or strokes.
Still, many doctors in the U.S. don’t follow this. A 2018 JAMA study found that 22% of dialysis patients in America still had hemoglobin levels above 11 g/dL-despite clear warnings. Some patients feel better at higher levels, but the science says the risk isn’t worth it.

What Happens When ESA Therapy Doesn’t Work
About 10% of CKD patients don’t respond to ESAs. This is called ESA hyporesponsiveness. The most common cause? Undiagnosed iron deficiency. Even if ferritin looks okay, inflammation can hide the problem. Other causes include chronic infection, aluminum toxicity (rare now), vitamin B12 or folate deficiency, or bone marrow damage.
When ESA doesn’t work, doctors don’t just crank up the dose. They look for the root cause. Maybe the patient needs more IV iron. Maybe they have an infection. Maybe they’re not taking their meds. A 62-year-old diabetic patient in a Mayo Clinic case report went from 8.2 to 10.5 g/dL in eight weeks after switching to weekly darbepoetin and 200 mg of IV iron sucrose. That’s the kind of turnaround possible when the right combination is used.
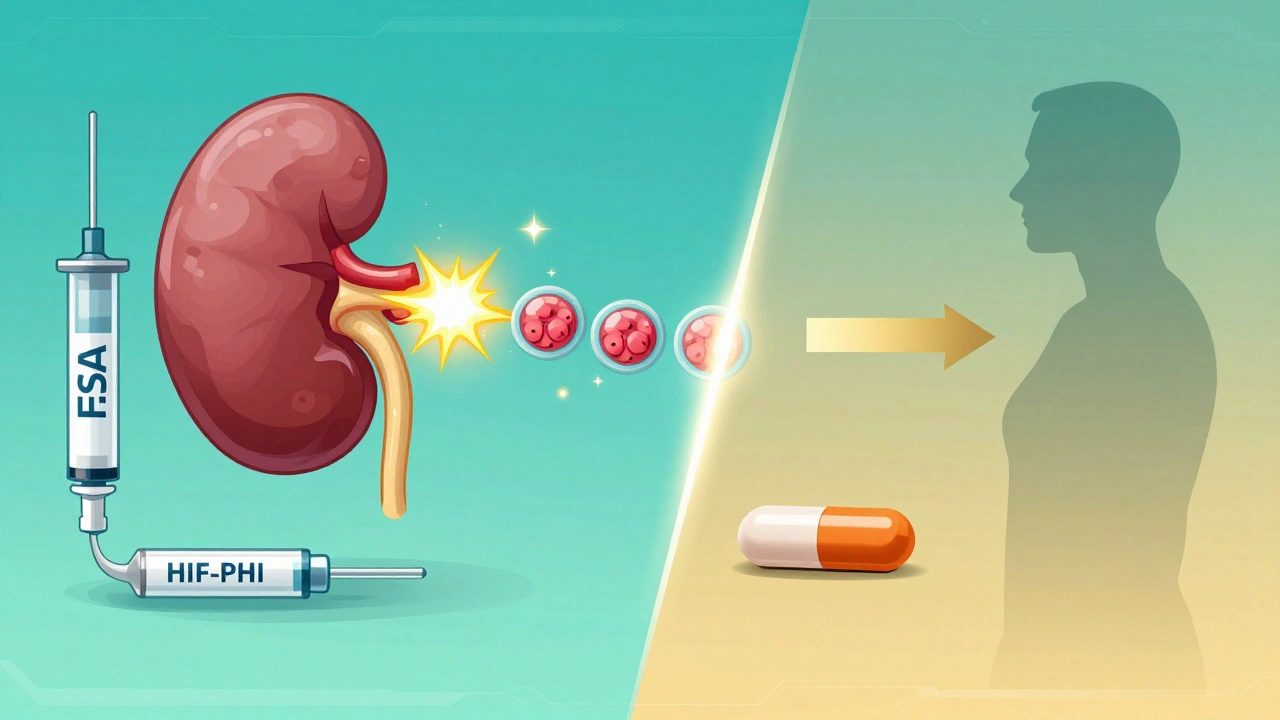
The New Kid on the Block: HIF-PHIs
For the first time since the 1990s, there’s a real alternative to injections. HIF-PHIs-like roxadustat and daprodustat-are oral drugs that trick your body into thinking it’s low on oxygen. That triggers natural erythropoietin production and improves iron use at the same time.
Roxadustat was approved in Japan in 2019, China in 2020, and finally in the U.S. in December 2023 under the brand name Evrenzo. Early data shows it raises hemoglobin as well as ESAs, but with fewer spikes in blood pressure and possibly better heart outcomes. It also helps iron move from storage into the blood, so you might need less IV iron.
But it’s not perfect. The FDA put a hold on roxadustat between 2018 and 2020 because of concerns about tumor growth in cancer patients. That’s why it’s not recommended for people with active cancer. It’s also more expensive than ESAs right now. Still, it’s a game-changer for patients who hate needles or struggle with IV iron access.
Real People, Real Results
Patients tell different stories. One woman on Reddit said, “I can finally play with my grandchildren without getting winded.” That’s the kind of quality-of-life improvement that matters. Another said, “The IV iron made me feel sick for hours, but I had energy for the first time in years.”
On the flip side, 32% of patients report worse high blood pressure after starting ESAs. One in four say they get injection site pain. And 45% of those getting IV iron complain of a metallic taste. These aren’t side effects to ignore. They’re signals that the treatment plan might need tweaking.
What Doctors Do Differently Now
Here’s the modern approach, step by step:
- Test: Check hemoglobin, ferritin, and TSAT. If hemoglobin is below 13 g/dL for men or 12 g/dL for women, you have anemia.
- Fix iron first: If ferritin is under 100, start IV iron. If ferritin is 100-500 and TSAT under 30%, start IV iron anyway.
- Wait 4-6 weeks: Let the iron work. Recheck hemoglobin.
- Start ESA only if needed: If hemoglobin is still below 10 g/dL after iron repletion, begin ESA therapy.
- Target 10-11.5 g/dL: Don’t chase higher numbers. More isn’t better.
- Monitor monthly: Hemoglobin, ferritin, TSAT. Adjust doses by 25% every 4 weeks based on trends.
Doctors now know that fixed targets don’t work. A 75-year-old with heart disease needs different goals than a 45-year-old who’s active and symptom-free. That’s why KDIGO says: treat the person, not the number.
The Future Is Personalized
Machine learning is starting to help. A pilot study at Mayo Clinic used AI to predict the right ESA dose for each patient, cutting dose variability by 22%. That means fewer ups and downs in hemoglobin and less risk of over- or under-treatment.
Next up? Minihepcidins-drugs that block the iron-blocking hormone hepcidin. If they work, we might finally be able to use oral iron effectively in CKD. And HIF-PHIs? They’ll keep growing. By 2028, they could be a $3.5 billion market.
For now, IV iron and ESAs remain the backbone of treatment. But the shift is clear: less injections, more pills; less one-size-fits-all, more personalization. And for patients, that means more energy, fewer hospital visits, and a real shot at living well-even with kidney disease.

Elliot Barrett
December 8, 2025 AT 21:12Why are we still using IV iron like it's 2010? Oral iron with hepcidin modulators is coming, and we're still sticking needles in people like they're lab rats.
precious amzy
December 10, 2025 AT 03:14One must question the epistemological foundations of treating hemoglobin as a metric rather than a symptom of systemic dysregulation. The KDIGO guidelines, while statistically robust, reduce the phenomenological experience of fatigue to a numerical target-an ontological error of the highest order.
Carina M
December 10, 2025 AT 11:10It is unconscionable that physicians continue to prescribe ESAs without first ensuring the patient has adequate access to nutritional counseling, sleep hygiene, and psychological support. Anemia is not merely a hematological condition-it is a moral failure of the healthcare system.
William Umstattd
December 10, 2025 AT 20:52Let me be perfectly clear: if your ferritin is below 100, you are not just iron-deficient-you are being neglected by a broken medical industrial complex. IV iron isn't a treatment-it's damage control for a system that refuses to fix the root cause: poverty, processed food, and pharmaceutical greed.
Ajit Kumar Singh
December 11, 2025 AT 15:54in india we dont even have IV iron in many hospitals and still people live with hgb 7.5 and smile because they have family to care for and no one to complain to. you all talk about guidelines like they are holy scripture but here we just try to keep them alive till the next moon
Maria Elisha
December 11, 2025 AT 18:22i just got my first iv iron and honestly? it felt like someone poured a can of soda into my vein. metallic taste for 3 hours. but then i could walk to my mailbox without stopping. worth it? yeah. but why does it have to suck so much?
Andrea Beilstein
December 13, 2025 AT 10:46we treat anemia like a machine that needs tuning but the body isn't a car it's a living system that remembers trauma and starvation and chronic stress. maybe we're not fixing the iron deficiency maybe we're just patching over the wound of systemic neglect
Lisa Whitesel
December 15, 2025 AT 02:21Anyone who says they feel better at Hgb 12 is either lying or has a tumor. The data is clear. Pushing past 11.5 is medical malpractice disguised as compassion.
Larry Lieberman
December 16, 2025 AT 02:10So HIF-PHIs are basically magic pills that trick your body into thinking it's on a mountain? 🤯 I'm so here for this. No needles? Yes please. 🙌
Sabrina Thurn
December 17, 2025 AT 12:00Just to clarify the clinical nuance: the shift toward HIF-PHIs isn't merely pharmacological-it's paradigmatic. By modulating hypoxia-inducible factors, we're not replacing erythropoietin; we're restoring endogenous regulatory homeostasis. This allows for physiological iron mobilization, reduces hepcidin-mediated blockade, and mitigates ESA-associated cardiovascular risk. The 2023 FDA approval of Evrenzo represents not just an advance, but a reorientation of therapeutic intent-from substitution to restoration.