Imagine skipping a human clinical trial for a generic drug - not because it’s risky, but because science says you don’t need it. That’s exactly what bioequivalence waivers let drug companies do. The U.S. Food and Drug Administration (FDA) won’t require expensive, time-consuming in vivo studies if the drug meets strict scientific criteria. For generic manufacturers, this isn’t just a shortcut - it’s a game-changer that saves millions and gets life-saving medicines to patients faster.
What Exactly Is a Bioequivalence Waiver?
A bioequivalence waiver, or biowaiver, is when the FDA accepts in vitro (lab-based) data instead of testing a drug in people. Normally, to prove a generic drug works like the brand-name version, companies must run in vivo studies: give the drug to volunteers, take blood samples over hours, and compare how much of the drug enters the bloodstream. These studies cost between $250,000 and $500,000 and take 6 to 12 months. But for certain drugs, the FDA says: “You don’t need to test in people. Just show us how quickly the tablet dissolves in lab conditions - and we’ll trust that it’ll behave the same in the body.” This isn’t a loophole. It’s based on decades of research showing that for some drugs, dissolution in the gut is the only thing that matters.The Science Behind the Waiver: BCS Classification
The key to getting a waiver lies in the Biopharmaceutics Classification System (BCS). This system groups drugs into four classes based on two properties: solubility (how well the drug dissolves in water) and permeability (how well it crosses the gut wall into the blood). The FDA grants waivers mostly for:- BCS Class I: High solubility, high permeability. These drugs dissolve easily and are absorbed completely. Examples include metoprolol, atenolol, and ranitidine.
- BCS Class III: High solubility, low permeability. These are trickier. The FDA only allows waivers if the generic has the exact same excipients (inactive ingredients) as the brand and the drug isn’t absorbed in a specific part of the gut.
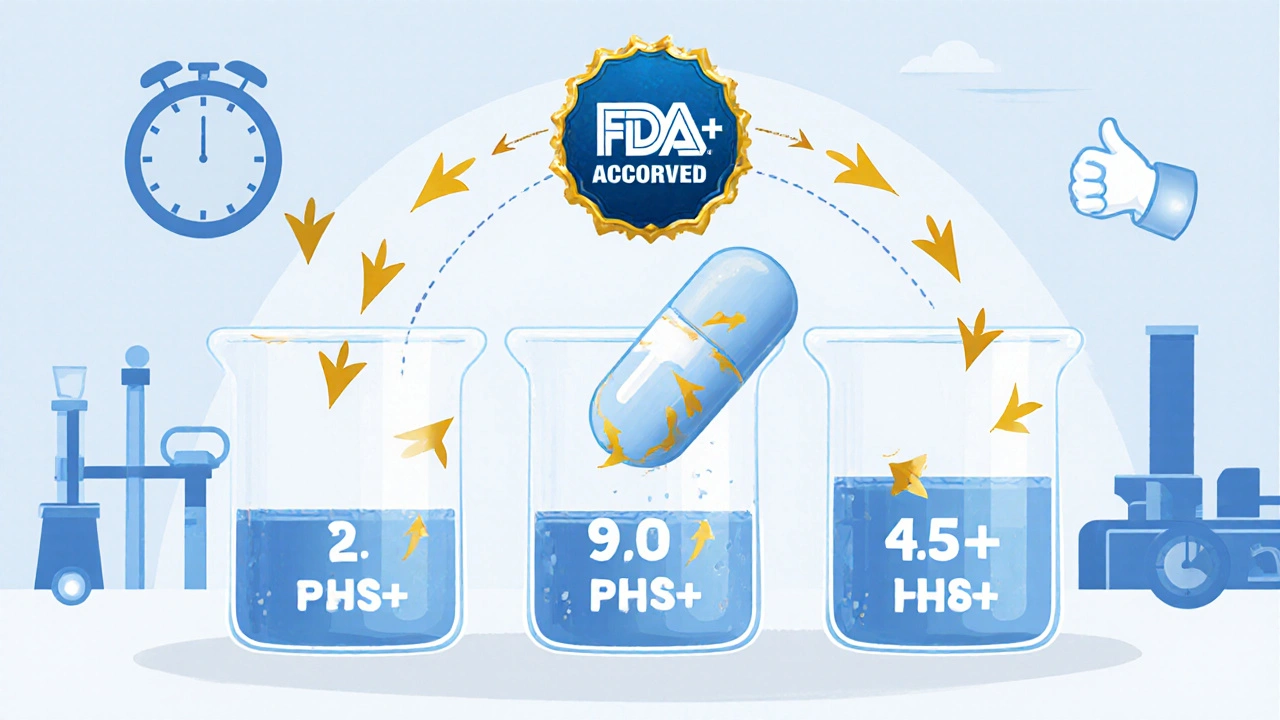
- The drug must dissolve at least 85% in 30 minutes in pH 1.2, 4.5, and 6.8 buffers - mimicking stomach and intestine conditions.
- The dissolution profiles of the generic and brand must match closely, with an f2 similarity factor of 50 or higher.
- The drug must have a dose number ≤ 1, meaning the dose is small enough to fully dissolve in the small intestine.
Why This Matters for Generic Drugs
The impact is huge. In fiscal year 2022, 18% of all Abbreviated New Drug Applications (ANDAs) for solid oral tablets used a biowaiver - up from 12% in 2018. That’s thousands of generic versions of common drugs approved without human trials. One generic company reported saving $4.2 million and cutting approval time by 8-10 months across 12 biowaiver submissions over three years. That’s not just cost savings - it’s faster access to affordable medicine. For patients on chronic meds like blood pressure or thyroid drugs, this means lower prices sooner. The FDA’s own data shows a 78% approval rate for complete biowaiver requests. But here’s the catch: if the dissolution method isn’t good enough, the application gets rejected. In fact, 35% of failed submissions were due to non-discriminatory dissolution testing - meaning the test couldn’t tell the difference between a good and bad formulation.
What Doesn’t Qualify for a Waiver?
Not all drugs can skip human studies. The FDA explicitly excludes:- Modified-release products - tablets that release drug slowly over hours. Their behavior is too complex to predict from dissolution alone.
- Narrow therapeutic index drugs - drugs where small changes in blood levels can cause toxicity or failure. Think warfarin, levothyroxine, or phenytoin. (Though there are exceptions - some antiepileptics are allowed under special rules.)
- BCS Class II and IV drugs - low solubility drugs like itraconazole or griseofulvin. Their absorption depends on complex factors like food, bile, and gut motility - things dissolution tests can’t capture.
How Companies Actually Get a Waiver Approved
Getting a waiver isn’t just filling out a form. It’s a technical marathon. Here’s what it takes:- Classify the drug - Use published data or run solubility and permeability tests. Permeability is often estimated using Caco-2 cell models or published human absorption data.
- Develop a dissolution method - Must be validated, physiologically relevant, and discriminatory. Use 12 tablets per batch. Sample at 10, 15, 20, 30, 45, and 60 minutes. Use USP apparatus I or II (basket or paddle) with pH 1.2, 4.5, and 6.8 buffers.
- Compare profiles - Use the f2 similarity factor formula. If it’s below 50, you’re not approved. Most companies run multiple batches to ensure consistency.
- Submit with justification - Include BCS classification data, dissolution profiles, method validation, and a clear argument that in vitro data is more reliable than in vivo for this drug.


Geoff Heredia
December 1, 2025 AT 07:27So let me get this straight - the FDA lets Big Pharma skip human trials and just ‘trust’ a tablet dissolves in a beaker? 🤨 Next they’ll say we don’t need to test if the moon is made of cheese - just measure how fast it crumbles in a microwave. This isn’t science, it’s corporate lobbying dressed up as efficiency. I bet the same people who approved this also said vaping was safe. 😏
Andrew Keh
December 2, 2025 AT 15:23This is actually a smart approach for certain drugs. If the science shows a drug behaves predictably in the body and the lab test proves it’s identical, why put people through blood draws? It saves time, money, and avoids unnecessary risk. The FDA isn’t cutting corners - they’re using data wisely.
Peter Lubem Ause
December 4, 2025 AT 07:51This is one of those moments where science finally catches up to common sense. For Class I drugs, dissolution is everything - the body doesn’t care if it’s brand or generic, only if the pill dissolves the same way. And yes, this saves millions. But more importantly, it gets life-saving meds to people who can’t afford brand names. This isn’t a loophole - it’s justice in a pill bottle. 🙌
jamie sigler
December 5, 2025 AT 05:36Yeah, sure. Let’s just trust a machine that dissolves pills in buffer solutions. Next they’ll replace doctors with AI chatbots and call it ‘personalized medicine.’ I mean, how hard is it to just… test on humans? Seems like everyone’s too lazy to do the right thing anymore.
Bernie Terrien
December 6, 2025 AT 20:17Biowaivers? More like ‘bribe-with-data’ waivers. The FDA’s got a 78% approval rate? That’s not rigor - that’s a rubber stamp for companies who can afford fancy dissolution labs. Meanwhile, your grandma’s blood pressure med? Still waiting on a human trial because the f2 score was 49.9. 😒
stephen idiado
December 8, 2025 AT 16:33BCS Class I? Please. You’re assuming gut absorption is linear. It’s not. It’s chaotic. Enzymes, microbiome, pH fluctuations - all ignored. This is reductionist nonsense masquerading as science. And ‘f2 > 50’? That’s not a threshold - it’s a suggestion written by someone who hasn’t touched a HPLC in a decade.
Subhash Singh
December 10, 2025 AT 05:52It is of paramount importance to note that the Biopharmaceutics Classification System has been validated through extensive in vivo-in vitro correlation studies spanning multiple decades. The application of biowaivers for BCS Class I and certain Class III drugs is not an arbitrary regulatory concession but a scientifically grounded paradigm shift that aligns with the principles of rational drug development.
Tina Dinh
December 11, 2025 AT 21:29YESSSS this is how we make medicine affordable!! 🎉💊 No more $5000 trials for a $5 pill! Let’s get more generics out there - people deserve access, not bureaucracy! 🙌 #BiowaiverWins
linda wood
December 12, 2025 AT 22:00Wow. So you’re telling me the FDA actually listens to science instead of just chasing profits? That’s… kinda beautiful? I mean, I expected them to say ‘nah, we need a human to swallow it first’ - but nope. They used data. And it’s working. I’m actually kinda moved.
LINDA PUSPITASARI
December 13, 2025 AT 16:56My cousin’s on levothyroxine and the price jumped 300% last year - if they can approve waivers for these drugs it could change everything 😭 I’ve seen people skip doses because they can’t afford it… this isn’t just policy it’s survival. Also f2 > 50 is legit - I work in pharma QA and trust me the method validation is brutal
gerardo beaudoin
December 14, 2025 AT 21:30Honestly, this makes total sense. If the pill dissolves the same way and the active ingredient is identical, why waste time and money testing on people? It’s like saying you need to test every single batch of aspirin in humans because… well, you’ve always done it that way. Time to update the playbook.
Joy Aniekwe
December 16, 2025 AT 10:48Oh great. So now we’re just trusting tablets to behave like they’re in a bathtub? And you call this ‘science’? Meanwhile, real people are getting sick because some lab technician misread a pH reading. I bet the FDA’s lunch budget is bigger than their patient safety team’s.
Latika Gupta
December 17, 2025 AT 00:21Wait - so you’re saying a tablet that dissolves in a beaker is safer than testing on humans? But what if the tablet is made in a factory in Bangladesh with unregulated ingredients? How do you know the generic isn’t just… sugar with a little bit of medicine? I’m not convinced. This feels dangerous.
Sohini Majumder
December 18, 2025 AT 13:00So… the FDA just said ‘eh, just dissolve it’? 😭 Like… are we really that lazy? I mean, I get it, money, blah blah - but what if the drug’s absorbed differently because of my gut flora? Or my age? Or I’m on a keto diet? This isn’t innovation - it’s a cop-out wrapped in a lab coat. #TrustTheScience? More like TrustTheSpreadsheet