Why Documenting Generic Substitutions Matters
Every time a pharmacist swaps a brand-name drug for a generic version, they’re making a decision that affects patient safety, insurance claims, and legal compliance. It’s not just about saving money-though that’s a big part of it. In 2022, generics made up 90% of all prescriptions filled in the U.S., but only 23% of total drug spending. That’s over $1.6 trillion saved over a decade. But behind every saved dollar is a record that needs to be accurate, complete, and timely. If you don’t document the substitution properly, you risk insurance denials, medication errors, or even patient harm-especially with drugs that have a narrow therapeutic index, like warfarin or lithium.
What Exactly Must Be Documented
There’s no single national rule, but across 48 states, pharmacists are required to record the same core details for every generic substitution:
- The brand name prescribed by the doctor
- The generic name dispensed
- The manufacturer or distributor of the generic product
- The lot number
- The expiration date
Some states add more. Oklahoma, for example, requires proof of patient or prescriber consent before any substitution. California’s SB 564, effective January 2024, demands real-time electronic documentation that prescribers can access immediately. In states with stricter rules, you might also need to note whether the patient agreed to the switch, or if the prescriber blocked substitution with a "Do Not Substitute" mark.
State Laws Vary-And It’s Complicated
There are 50 different sets of rules. Twenty-seven states let pharmacists substitute generics without asking the patient. Fourteen states require the patient to give explicit consent before the switch. Nine use a mix of both. Why does this matter? Because if you work for a national pharmacy chain, you can’t use one system for all locations. You need custom workflows for each state.
States that require consent also tend to have higher prescription costs-$15.35 more per script on average-because patients sometimes stick with the brand-name drug even when a cheaper generic is available. Meanwhile, 17 states have special rules for Narrow Therapeutic Index (NTI) drugs. These are medications where even tiny changes in blood levels can cause serious side effects. For these, many states require extra steps: notify the prescriber, get written consent, and document the reason why the substitution was made.
Electronic Systems Aren’t Always Ready
Most pharmacies use electronic health records (EHRs) or pharmacy management systems like Epic or Cerner. But these systems weren’t built for 50 different state laws. A 2023 update from Epic Systems showed that 32% of pharmacies had to build custom fields or workflows just to meet their state’s documentation rules. That means extra training, extra time, and extra frustration for staff.
Some pharmacists report adding 30 seconds per prescription just to enter all the required fields. That adds up. But skipping steps is risky. One case in the Journal of the American Pharmacists Association found that poor documentation of a warfarin substitution led to a patient’s hospitalization due to uncontrolled INR levels. Proper records didn’t just prevent that-they helped identify the error after it happened.
When and How Quickly Must You Document?
Timing matters. Forty-one states require documentation to be completed within 24 hours of dispensing. Some require it before the patient leaves the pharmacy. Delayed entries increase the chance of mistakes, especially if the pharmacist is juggling multiple prescriptions or a busy shift.
Electronic documentation is now the norm. In 2023, 98% of chain pharmacies and 87% of independent pharmacies used digital systems to track substitutions. Paper logs are fading out-not because they’re illegal, but because they’re slow, hard to audit, and don’t integrate with insurance billing systems. If your system can’t auto-populate the lot number or expiration date from the inventory, you’re doing it the hard way.
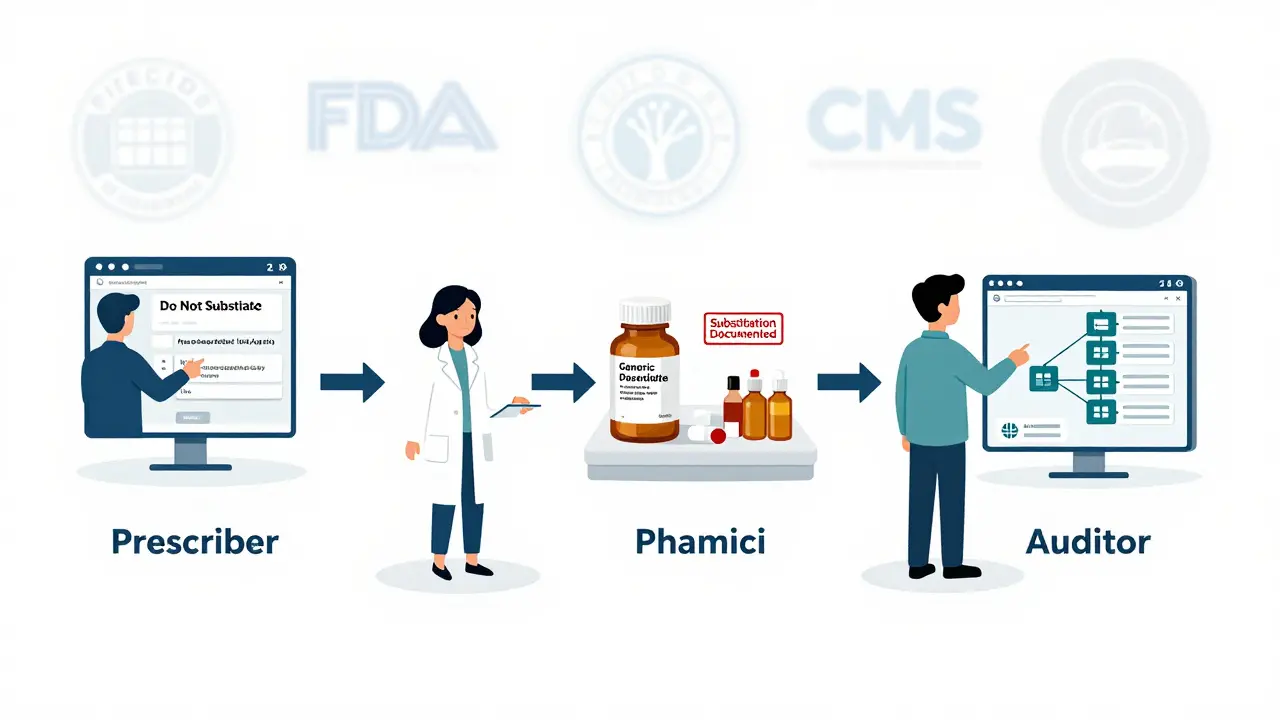
Why This Isn’t Just a Pharmacy Problem
The American Medical Association says doctors should document when they prescribe a brand-name drug for medical necessity-like when a patient has had a bad reaction to a generic in the past. But without clear communication between prescriber and pharmacist, those notes get lost. That’s why some states now require prescribers to electronically flag "Brand Necessary" in e-prescribing systems. If the pharmacist sees that flag, they can’t substitute, even if the insurance wants them to.
The World Medical Association also recommends that once a patient is stable on a drug-brand or generic-no changes should be made without the prescriber’s approval. That’s especially true for chronic conditions like epilepsy, thyroid disorders, or mental health treatments. Switching brands mid-treatment can destabilize a patient, even if the drugs are technically "therapeutically equivalent." Documentation helps trace back why a change happened-and whether it caused a problem.
Real-World Impact: Data Proves It Works
It’s not just about avoiding mistakes. Good documentation saves lives and money. A 2022 study across 150 community pharmacies found that when substitution decisions were fully documented, medication errors dropped by 17.3% in just six months. The American Pharmacists Association’s 2022 survey showed that 23% of pharmacists had prevented an adverse event because they had a clear record of what was dispensed.
And it’s not just clinical outcomes. Insurance companies audit substitution records constantly. If you can’t prove you followed state law, claims get denied. Pharmacists report that clean documentation cuts down on claim rejections by up to 40%. That means faster reimbursement, fewer phone calls from billing departments, and less stress for everyone involved.
What’s Changing in 2025
The FDA’s Generic Drug User Fee Amendments (GDUFA III), updated in 2022, now require manufacturers to submit more detailed bioequivalence data for complex generics-like extended-release or inhaled drugs. That means pharmacists may soon see more variation in generic products, even if they have the same name. More data means more need for accurate documentation.
California’s real-time electronic reporting law is setting a new standard. Other states are watching. The Model State Pharmacy Act, updated in 2022, now recommends uniform documentation rules-and 12 states have already adopted them. The Centers for Medicare & Medicaid Services (CMS) also tightened requirements for Part D drugs in 2022, mandating clear substitution notes for audits.
Looking ahead, blockchain pilots are being tested to track substitutions end-to-end. A 2023 pilot by the National Pharmaceutical Council showed a 22% drop in documentation errors when substitution records were stored on a tamper-proof digital ledger. The Department of Health and Human Services is drafting national guidelines expected in mid-2024. If they pass, we could see a big reduction in the current patchwork of state rules.
What Pharmacists Need to Know Today
If you’re a pharmacist, here’s your checklist:
- Know your state’s substitution law-don’t assume it’s the same as your neighbor’s.
- Use your pharmacy system’s built-in substitution module. Don’t rely on handwritten notes.
- Document everything within 24 hours. If you wait, you’ll forget details.
- For NTI drugs, always check if your state requires extra steps-consent, prescriber notification, or both.
- When a prescriber writes "Do Not Substitute," respect it. No exceptions.
- Train new staff. It takes 4 to 6 weeks to get comfortable with state-specific rules.
There’s no shortcut. But good documentation isn’t just compliance-it’s protection. For your patient. For your license. For your pharmacy.
Where to Find Help
The National Community Pharmacists Association (NCPA) offers a free, updated online tool that cross-references state laws with documentation requirements. It’s updated quarterly and includes direct links to state pharmacy board regulations. If you’re unsure whether you need consent, or whether your system is compliant, start there.
Do I need patient consent to substitute a generic drug?
It depends on your state. Fourteen states require explicit patient consent before substituting a brand-name drug with a generic. Twenty-seven states allow pharmacists to substitute without asking. Nine states use a hybrid model. Always check your state’s pharmacy board regulations. If the prescription has a "Do Not Substitute" note from the prescriber, you cannot substitute regardless of state law.
What if I make a mistake in documenting a substitution?
If you catch the error before the patient leaves, correct it immediately in your system and note the correction. If the error is discovered later-say, during an audit or after an adverse event-you must report it to your pharmacy’s compliance officer. In some cases, you may need to notify the patient and the prescriber. Documentation errors are a leading cause of insurance claim denials and can lead to disciplinary action if they’re repeated or involve high-risk drugs like warfarin or digoxin.
Are all generics truly interchangeable?
The FDA requires generics to be bioequivalent-meaning they deliver the same amount of active ingredient into the bloodstream within a narrow range (80-125%). But bioequivalence doesn’t always mean identical clinical effect. For drugs with a narrow therapeutic index (NTI), even small differences in absorption can cause problems. That’s why 17 states have special rules for NTI drugs. Always check if the drug is classified as NTI in your state’s formulary, and follow additional documentation steps if required.
Can I substitute a generic if the prescriber didn’t specify brand or generic?
Yes, in most states. If the prescription just lists the drug name without specifying brand or generic, you’re allowed to dispense an FDA-approved generic unless the prescription says "Dispense as Written" or "Do Not Substitute." Always confirm the prescriber’s intent. If you’re unsure, call the prescriber’s office. It takes 30 seconds and prevents a potential error.
Do I need to document substitutions for Medicare Part D patients?
Yes. CMS requires clear documentation of substitutions for all Part D drugs, including the name of the generic dispensed, the manufacturer, and the lot number. This is for audit purposes and to track drug utilization patterns. Failure to document properly can result in denied claims and financial penalties for the pharmacy. Make sure your pharmacy system has a dedicated field for Part D substitution records.
How long should I keep substitution records?
Most states require pharmacy records to be kept for at least two years from the date of dispensing. Some states, like New York, require five years. Electronic records must be stored in a secure, retrievable format. Paper records should be kept in a locked cabinet. Always check your state’s pharmacy board rules. In case of litigation or audit, you may need to produce these records years later.


Paul Ong
January 1, 2026 AT 17:15Donna Peplinskie
January 2, 2026 AT 18:45Alex Warden
January 3, 2026 AT 14:14Olukayode Oguntulu
January 5, 2026 AT 12:20jaspreet sandhu
January 6, 2026 AT 04:26Richard Thomas
January 7, 2026 AT 06:59LIZETH DE PACHECO
January 8, 2026 AT 11:41Andy Heinlein
January 10, 2026 AT 05:53Bill Medley
January 10, 2026 AT 21:42