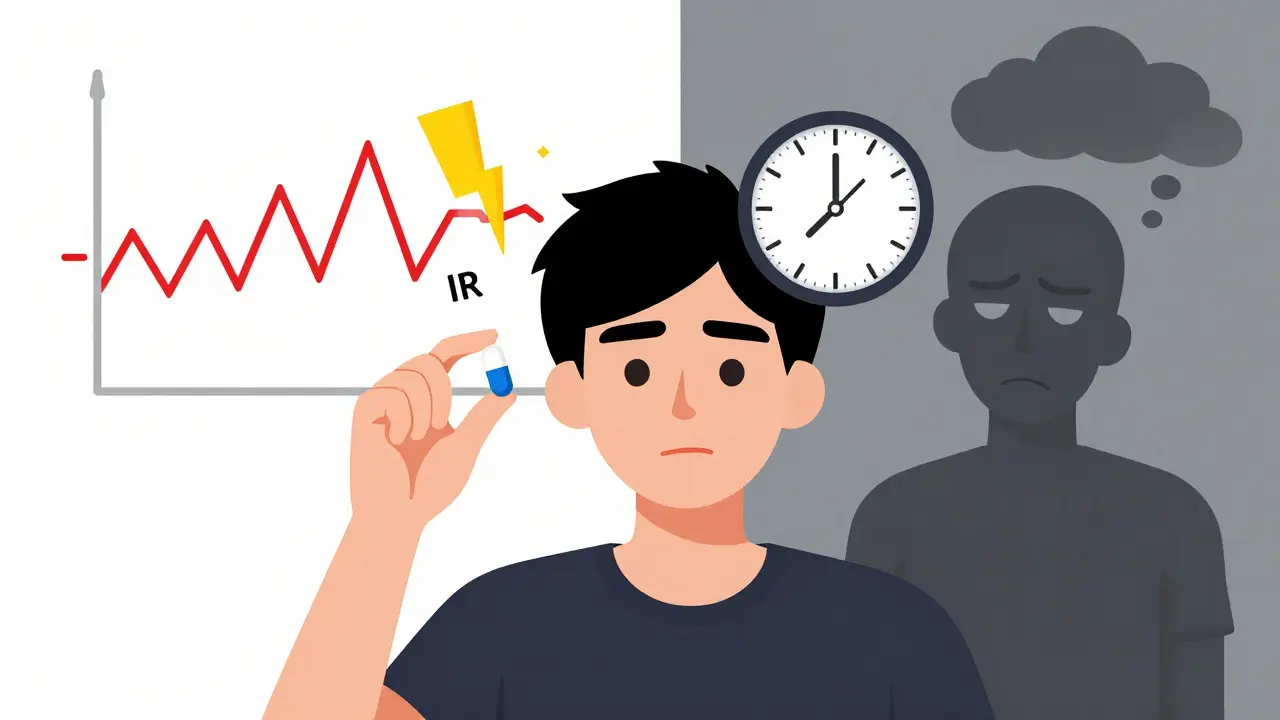
Imagine taking a pill for your depression, and within an hour, you feel like a new person-energized, focused, calm. Then, four hours later, you’re back to feeling empty, irritable, exhausted. That’s what happens with immediate-release medications. Now imagine taking one pill in the morning that holds steady all day, no crashes, no spikes, just steady relief. That’s the promise of extended-release. But here’s the catch: neither is better outright. Choosing the wrong one can mean the difference between stable health and a trip to the ER.
How These Two Types Work
Immediate-release (IR) pills are simple. They dissolve fast. Within 15 to 30 minutes after swallowing, your body starts absorbing the full dose. Peak levels hit in under two hours. That’s great if you need fast relief-like for sudden pain, a panic attack, or a migraine. But it also means the drug fades quickly. You’re chasing the high, then crashing. That’s why IR versions often need to be taken three or four times a day. Extended-release (ER), on the other hand, is engineered. These aren’t just regular pills with a delay. They use smart tech: hydrogel matrices that slowly swell and release the drug, osmotic pumps that push medication out like a tiny drip system, or layered tablets that shed their contents over time. The goal? Keep drug levels steady-between the minimum dose that works and the maximum your body can safely handle-for 12 to 24 hours. That’s why you only need one or two doses a day. Take bupropion, an antidepressant. The IR version can spike blood levels to 600 ng/mL within two hours. That’s above the 350 ng/mL seizure threshold. The ER version? It creeps up to 150 ng/mL and holds there. No spikes. No crashes. Just safety.When Speed Matters
Not every condition can wait. If you’re having a sudden flare-up of pain, anxiety, or asthma, you need the drug to act now. That’s where immediate-release wins. For example, someone with chronic back pain might take an ER opioid at night to sleep through the night. But if they twist wrong during the day and get sharp, shooting pain? They need an IR tablet right then. Waiting 30 minutes for an ER pill to kick in isn’t an option-it’s dangerous. Same goes for ADHD. Adderall IR gives a quick boost for a presentation or a tough meeting. But if you’re taking it every day for school or work, the IR version means midday crashes, mood swings, and the awkwardness of needing to take a pill at lunch. Adderall XR? One pill. Twelve hours of steady focus. No midday pharmacy run. The American Psychiatric Association recommends ER for long-term management of depression, bipolar disorder, and schizophrenia-not because it’s stronger, but because it’s steadier. Stable blood levels mean fewer side effects like insomnia, nausea, or jitteriness that come from rollercoaster drug spikes.The Hidden Risks of ER
Extended-release sounds perfect-until something goes wrong. First, ER pills can’t be crushed, split, or chewed. Ever. If you break open a Concerta tablet, you’re not getting a half-dose-you’re getting the full 36mg all at once. That’s a known cause of overdose. The FDA issued a safety alert in 2020 after dozens of ER opioid overdoses from patients who crushed their pills to get high. The same goes for Venlafaxine XR, Metformin ER, and dozens of others. 92% of ER formulations are designed to be taken whole. If the pill isn’t scored, don’t cut it. Second, ER drugs take longer to work. You don’t feel better right away. It can take 2 to 4 hours to reach therapeutic levels. That’s confusing for patients. Many think, “This isn’t working,” and take another pill. That’s how accidental overdoses happen. A 2022 GoodRx survey found 41% of ER users took extra doses because they didn’t feel effects fast enough. Nine percent ended up in the hospital with nausea, dizziness, or worse. Third, ER medications are harder to reverse in emergencies. If someone overdoses on IR bupropion, the drug clears from the body in 6 to 8 hours. But ER bupropion? It keeps releasing for 24 to 48 hours. Hospital stays are 2 to 3 times longer. The National Poison Data System reports ER overdoses are more complex, more dangerous, and more expensive to treat.
Adherence and Cost: The Real-World Trade-Off
One of the biggest reasons doctors push ER is adherence. People forget pills. They skip doses. They get tired of taking medicine three times a day. A 2022 JAMA study tracked 15,000 people on blood pressure meds. Those on ER versions had a 78% adherence rate. IR users? Only 56%. That’s a 22-point gap. That’s not just convenience-it’s fewer heart attacks, fewer strokes, fewer hospitalizations. But ER isn’t cheap. Adderall XR costs $350 to $450 for 30 capsules. Adderall IR? $280 to $380. That’s a 15-25% premium. For people paying out of pocket, that matters. Some switch to IR to save money-and then struggle with side effects or missed doses. Patient reviews tell the real story. On Reddit, someone wrote: “I keep 5mg IR tabs for presentations. XR keeps me going, but IR gives me that laser focus when I need it.” That’s smart. It’s not about picking one. It’s about using both wisely.Who Gets Which?
Here’s the practical breakdown:- Choose ER if: You’re on long-term meds for depression, anxiety, ADHD, high blood pressure, diabetes, or chronic pain. You want fewer doses. You hate midday pill breaks. You’ve had side effects from IR spikes.
- Choose IR if: You need fast relief-pain, panic, seizures, migraines. You’re starting a new drug and your doctor is titrating the dose. You’re on a tight budget and can manage multiple daily doses.
- Use both if: Your doctor prescribes ER for daily control and IR for breakthrough symptoms. This is common in chronic pain, ADHD, and bipolar disorder.
What You Need to Ask Your Pharmacist
Before you leave the pharmacy, ask these three questions:- Is this tablet scored? If not, don’t split it.
- How long until I feel the full effect? Don’t assume it’s instant.
- What happens if I miss a dose? With ER, skipping one day can cause withdrawal. With IR, you just feel the symptoms come back.

What’s Next?
The future of pills is getting smarter. MIT researchers are testing 3D-printed “polypills” that release different drugs at precise times-like one for morning, one for afternoon, one for night-all in one tablet. Drug companies are also adding abuse-deterrent tech, like gels that form when you try to crush the pill. These are promising. But right now, the choice between ER and IR is still yours-and your doctor’s-to make wisely. It’s not about what’s newer or pricier. It’s about what matches your life, your body, and your risks.Don’t Guess. Know.
If you’re on an ER medication, read the label. Look for words like XR, SR, CR, or DR. If you see them, treat that pill like a precision tool-not a candy. Don’t crush it. Don’t skip doses. Don’t double up if you don’t feel it right away. And if you’re on IR, don’t feel like you’re doing something wrong for needing to take it more often. Sometimes, speed is the safest option. Your body doesn’t care about marketing. It cares about steady levels, clear instructions, and respect for the science behind the pill.Can I split my extended-release pill in half?
Only if the pill is specifically scored and the manufacturer says it’s safe. Most extended-release pills-like Venlafaxine XR, Metformin ER, or Concerta-are not meant to be split. Crushing or splitting them can release the full dose at once, leading to dangerous spikes in drug levels. Always check the label or ask your pharmacist.
Why do I feel worse when I switch from IR to ER?
It’s not uncommon. ER versions take longer to build up in your system-often 7 to 10 days to reach steady levels. If you switch cold turkey, your body may go through a temporary dip in medication, causing withdrawal-like symptoms. Always ask your doctor about a gradual transition. Don’t stop IR abruptly unless instructed.
Is extended-release better for mental health?
For long-term management, yes. ER formulations reduce the peaks and valleys in blood levels that cause side effects like insomnia, anxiety, or mood swings. Studies show patients on ER antidepressants report fewer side effects and better adherence. But for acute episodes or when adjusting doses, IR is still essential. It’s not about one being better-it’s about using the right tool for the right moment.
What should I do if I accidentally crush an ER pill?
Call poison control immediately (in New Zealand, dial 0800 764 766). Even if you feel fine, ER pills release their full dose over hours. Crushing them can cause overdose symptoms hours later. Don’t wait for symptoms to appear. Save the pill packaging-it helps medical staff identify the drug and its release mechanism.
Can I take ER and IR versions together?
Yes-but only under a doctor’s direction. Some people use ER for daily control and IR for breakthrough symptoms, like sudden anxiety or pain. This is common with ADHD and chronic pain meds. Never combine them on your own. Taking extra IR on top of ER can lead to dangerous drug buildup. Always check with your prescriber.
Why do ER pills cost more?
Because they’re more complex to make. ER formulations require special coatings, matrices, or delivery systems that add to production costs. They also undergo stricter FDA testing to prove they release drug steadily over time. While the upfront cost is higher, many patients save money long-term by avoiding hospital visits from missed doses or side effects.

SHAKTI BHARDWAJ
December 28, 2025 AT 11:32so i took my er bupropion like a candy yesterday bc i was mad and now im in the er and theyre like oh u crushed it?? yeah i thought it was a skittle lmao
Matthew Ingersoll
December 28, 2025 AT 20:56The science behind extended-release formulations is genuinely impressive. The osmotic pump technology alone represents decades of pharmaceutical engineering. What matters most is patient education-too many people treat pills like they’re interchangeable snacks.
jesse chen
December 29, 2025 AT 15:44I’ve been on ER sertraline for five years now, and I can’t believe how much my anxiety has stabilized. Before, I’d get jittery by 3 p.m., couldn’t sleep, and felt like I was on a rollercoaster. Now? I wake up, take one pill, and just live. No more counting hours until the next dose. Also-never split a pill unless it’s scored. My pharmacist nearly had a heart attack when I asked if I could cut mine in half.
Alex Ragen
December 31, 2025 AT 13:15One might argue that the very notion of ‘steady-state pharmacokinetics’ is a bourgeois construct-a capitalist illusion designed to pacify the masses with the myth of control. We are not machines to be calibrated with timed-release pellets. The body knows its own rhythm. Why should a pill dictate the cadence of my soul? The ER pill is a metaphor for modern alienation: slow, silent, and suffocating in its false consistency.
Lori Anne Franklin
December 31, 2025 AT 23:46My dad switched from IR to ER for his blood pressure and now he’s actually remembering to take it! He used to skip doses like it was a game. Now he says it’s just easier. Also, side effects? Way less dizziness. I’m so glad he finally listened to the doc 😊
Sarah Holmes
January 2, 2026 AT 16:16Let me be perfectly clear: the pharmaceutical industry has weaponized extended-release technology to extend patent life, inflate prices, and manipulate patient dependency. The FDA’s approval process is a charade. The fact that you’re being told to ‘trust the science’ while paying $400 for a month’s supply of XR Adderall is not medicine-it’s exploitation. And if you’re taking it without a prescription? You’re not a user-you’re a pawn.
Jay Ara
January 4, 2026 AT 12:57bro i used to take ir adderall 3x a day and i was wrecked. switched to xr and now i can actually finish a book. no more lunchtime panic runs to the pharmacy. just one pill and i’m good. dont overthink it. your brain will thank you.
Michael Bond
January 6, 2026 AT 11:38ER for daily use. IR for emergencies. Simple.
Kuldipsinh Rathod
January 8, 2026 AT 01:11my cousin took her er metformin and crushed it bc she thought it’d work faster… ended up in the hospital with low blood sugar. never do that. just dont.
carissa projo
January 9, 2026 AT 10:11There’s something quietly revolutionary about the idea that healing doesn’t have to be frantic. We live in a world that rewards speed-fast food, fast replies, fast fixes. But the extended-release pill whispers: ‘You don’t need to rush. You don’t need to chase. Just let it unfold.’ It’s not just chemistry-it’s a philosophy of patience. And maybe, just maybe, that’s the most powerful medicine of all.
josue robert figueroa salazar
January 10, 2026 AT 19:33Everyone’s acting like ER is some miracle cure. Newsflash: it’s just a slower way to get high. And if you’re not crushing it, you’re just wasting money. The real question is why we’re even letting Big Pharma control our neurotransmitters like this.
david jackson
January 12, 2026 AT 06:36Okay, so imagine this: you’re a pill. Not just any pill-no, you’re a masterpiece of micro-engineering. Your outer shell is a fortress. Inside, there’s a labyrinth of hydrogels, osmotic chambers, timed-release membranes-all designed to drip-feed your active ingredient into the bloodstream like a slow, steady river. You’re not meant to be crushed. You’re not meant to be split. You’re meant to be respected. And yet-humans treat you like a gumball. They chew you. They grind you. They dissolve you in vodka. And then they wonder why they feel like they’ve been hit by a truck three hours later. The tragedy isn’t the overdose. The tragedy is that no one ever asked you, the pill, how you wanted to be treated. You just… kept releasing. Quietly. Patiently. Until the system broke. And now, you’re just another statistic in a hospital chart. And nobody remembers your name.