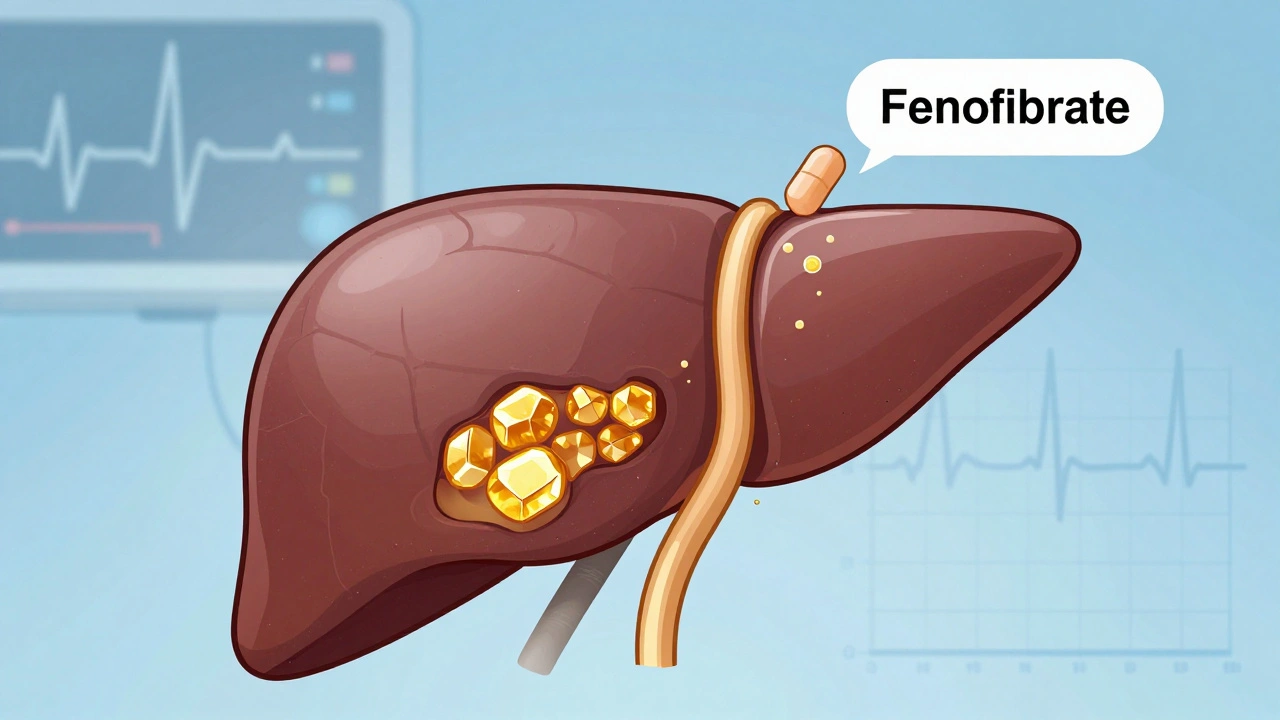
Many people take fenofibrate to lower triglycerides and raise good cholesterol, but few realize it can increase the risk of gallstones. If you’ve been prescribed this medication and suddenly feel pain under your right rib, it’s not just coincidence. Fenofibrate doesn’t cause gallstones overnight, but over time, it changes how your body handles bile - and that’s where the problem starts.
What Fenofibrate Does to Your Liver and Gallbladder
Fenofibrate is a fibrate drug, part of a class that activates a protein called PPAR-alpha. This tells your liver to burn more fat and make less triglyceride. That’s good for your heart. But it also makes your liver pump more cholesterol into bile. Bile is stored in your gallbladder until you eat, then released to help digest fats. When bile gets too rich in cholesterol, it starts to harden - forming crystals, then stones.
Studies show that people taking fenofibrate have a 2-3 times higher chance of developing gallstones compared to those not on the drug. A 2021 analysis of over 12,000 patients in the UK’s primary care database found that those on fenofibrate were significantly more likely to be diagnosed with gallstones within two years of starting treatment. The risk isn’t huge for everyone, but it’s real - and it’s avoidable if you know the signs.
Why Some People Get Gallstones and Others Don’t
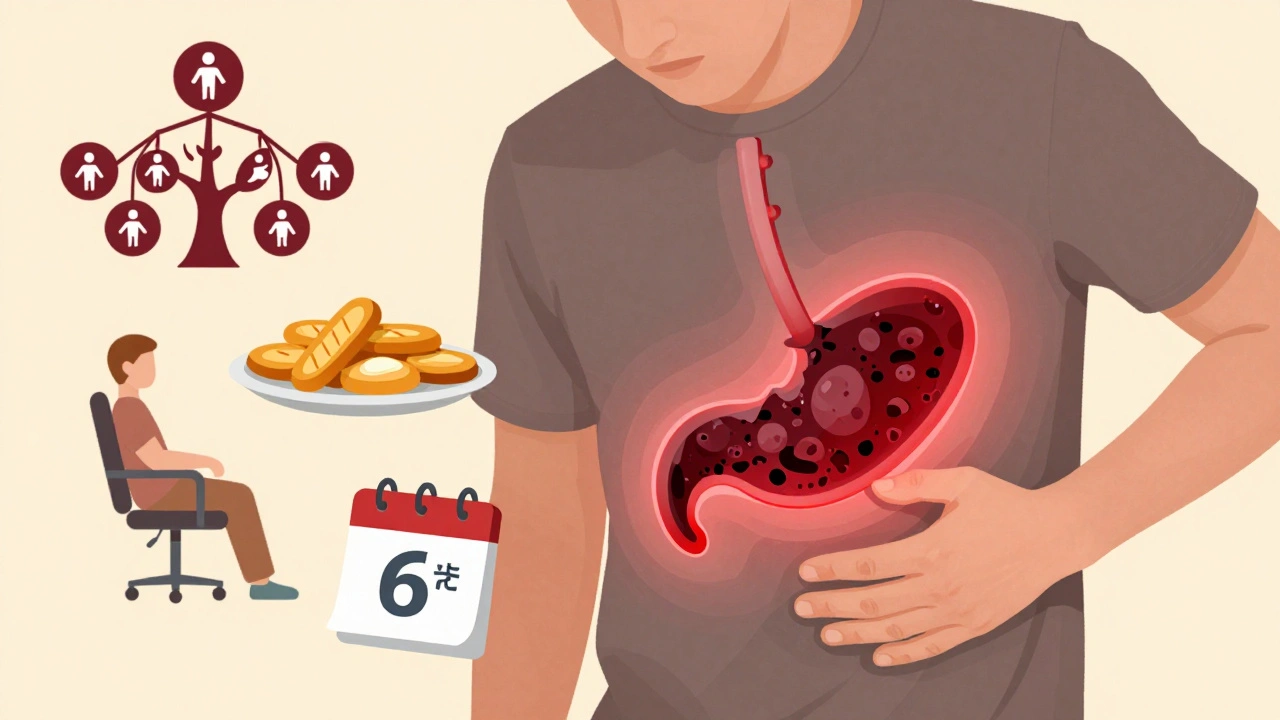
Not everyone on fenofibrate ends up with gallstones. Why? It comes down to three things: your body’s natural bile composition, how much fat you eat, and whether you already had silent gallstones before starting the drug.
People with a genetic tendency to make cholesterol-rich bile - often called "cholesterol hypersecretors" - are at the highest risk. If your family has a history of gallbladder surgery, you’re more likely to be one of them. Also, if you’re overweight or have metabolic syndrome, your liver is already working harder to process fats. Fenofibrate adds fuel to that fire.
Here’s what the data says: in clinical trials, gallstones developed in about 5% of patients taking fenofibrate over 5 years. That sounds low, but for someone already at risk, it’s a big jump. And here’s the catch - most of those stones were silent at first. No pain. No symptoms. Just quietly growing.
The Silent Progression of Gallstones
Gallstones don’t always hurt. In fact, up to 80% of people with them never feel anything. But when they do, it’s sudden and brutal. Pain under the right rib, often after a fatty meal. Nausea. Vomiting. Sometimes fever. That’s a gallbladder attack - and it’s not something you can treat with antacids.
If you’re on fenofibrate and start having these symptoms, don’t wait. Get an ultrasound. It’s quick, painless, and tells you everything you need to know. Many doctors don’t think to check for gallstones unless the patient is in obvious pain. But if you’re on fenofibrate, it’s worth asking. Early detection means you can avoid emergency surgery.
What to Do If You’re Taking Fenofibrate
Don’t stop your medication without talking to your doctor. But do take these steps:
- Watch for symptoms. Right upper belly pain, especially after meals, is the biggest red flag.
- Get screened if you’re high-risk. If you’re over 50, female, overweight, or have a family history of gallbladder disease, ask for an ultrasound after 6-12 months on fenofibrate.
- Watch your diet. Avoid fried foods, heavy cream, butter, and fatty meats. These trigger bile release and can push stones into the ducts.
- Stay active. Walking 30 minutes a day helps your gallbladder empty regularly. Sitting all day lets bile sit and thicken.
- Consider alternatives. If you’re at high risk and your triglycerides aren’t dangerously high, your doctor might switch you to a different lipid-lowering drug, like ezetimibe or a low-dose statin.
One 2023 study in the Journal of Clinical Lipidology followed 300 patients on fenofibrate. Half got regular ultrasounds and dietary advice. The other half didn’t. The screened group had 60% fewer gallbladder surgeries. Simple monitoring made a huge difference.
Alternatives to Fenofibrate
If your triglycerides are above 500 mg/dL, fenofibrate is still the best option. But if they’re only mildly elevated - say, between 200 and 499 - you might not need it at all. Lifestyle changes can do the job:
- Reduce sugar and refined carbs - these turn into triglycerides in your liver.
- Get omega-3s from fish, not pills - two servings of salmon or sardines a week can lower triglycerides by 20-30%.
- Lose 5-10% of your body weight - even a small drop can cut triglycerides by half.
For people who still need medication, ezetimibe lowers cholesterol without affecting bile. Statins like atorvastatin are safer for the gallbladder and often work well when combined with lifestyle changes. Talk to your doctor about whether switching makes sense for you.

What Happens If You Do Get Gallstones
If you develop gallstones, your doctor will likely recommend surgery - removing the gallbladder. It’s one of the most common surgeries in the world. Most people go home the same day. Afterward, digestion changes slightly - you might have looser stools after fatty meals - but your body adapts quickly.
Some people try to dissolve stones with pills like ursodiol. But that only works for small, cholesterol-based stones, and it takes months. Fenofibrate-induced stones are often too large or too numerous for this to help. Surgery is faster, safer, and more reliable.
And here’s something most people don’t know: once your gallbladder is gone, your risk of future gallstones drops to zero. No more worrying about fenofibrate triggering another attack.
Bottom Line: Knowledge Is Your Best Defense
Fenofibrate saves lives by reducing heart attack risk in people with high triglycerides. But it’s not risk-free. The trade-off - a slightly higher chance of gallstones - is worth it for some, but not for others. The key is knowing your personal risk and staying alert.
If you’re on fenofibrate, don’t ignore belly pain. Don’t assume it’s indigestion. Get checked. Eat smarter. Move more. Talk to your doctor about alternatives. You don’t have to choose between heart health and gallbladder health - you just need to be informed.
Can fenofibrate cause gallbladder pain?
Yes. Fenofibrate increases cholesterol in bile, which can lead to gallstone formation. These stones can block ducts and cause sudden, intense pain under the right rib - often after eating fatty foods. This isn’t just gas or heartburn - it’s a gallbladder attack.
How common are gallstones with fenofibrate?
About 5% of people taking fenofibrate develop gallstones over five years. That’s 2-3 times higher than those not on the drug. Risk is higher in women, people over 50, those with obesity, and those with a family history of gallbladder disease.
Should I stop fenofibrate if I develop gallstones?
Don’t stop on your own. Talk to your doctor. If you develop symptomatic gallstones, you’ll likely need surgery. After removal, your doctor may switch you to a different lipid-lowering drug like ezetimibe or a statin. Fenofibrate can often be safely restarted after gallbladder removal since the stone-forming environment is gone.
Can diet prevent gallstones while on fenofibrate?
Yes. Avoiding fried foods, butter, cream, and fatty meats reduces the chance of triggering gallbladder attacks. Eating regular, smaller meals helps your gallbladder empty consistently. High-fiber foods like oats, beans, and vegetables also help bind cholesterol in the gut. But diet alone won’t reverse stone formation if your bile is already too rich in cholesterol.
Is there a blood test to check for gallstone risk?
No direct blood test exists. But your doctor can look at your liver enzymes, cholesterol levels, and triglycerides to assess risk. If your LDL is high and HDL is low, your bile may be more prone to forming stones. An ultrasound is the only reliable way to confirm gallstones.
Can fenofibrate dissolve existing gallstones?
No. Fenofibrate actually makes gallstones more likely to form by increasing cholesterol in bile. It doesn’t dissolve them. Medications like ursodiol can dissolve small, cholesterol-based stones - but they’re rarely effective for fenofibrate-induced stones, which are often larger and more numerous.
Are gallstones dangerous if they don’t cause symptoms?
Silent gallstones usually aren’t dangerous. But they can become a problem if they move and block a duct. That can lead to infection, pancreatitis, or jaundice. For people on fenofibrate, the risk of future complications is higher, so monitoring is recommended even if you feel fine.

Linda Migdal
December 1, 2025 AT 17:59Fenofibrate is a pharmaceutical Trojan horse. The FDA knew this. The lipidologists knew this. But the pharma reps kept handing out free samples like candy. Gallstones aren't a side effect-they're a feature engineered by profit-driven pharmacology. Your liver isn't broken, it's being exploited. And now you're paying for it with your gallbladder.
They'll tell you it's 'rare.' But when 5% of a population of 10 million gets cholecystectomies because of a drug that was never properly monitored? That's not rare. That's negligence dressed up as science.
Stop trusting your doctor to catch this. Get the ultrasound. Now. Don't wait for pain. Silent stones don't whisper-they explode.
And if your doctor says 'it's fine'-find a new one. This isn't 1998 anymore. We have imaging. We have data. We have zero excuse for ignorance.
Tommy Walton
December 3, 2025 AT 15:11PPAR-alpha activation → bile cholesterol flux → crystallization cascade 🤯
It’s not a drug. It’s a metabolic ballet gone wrong. Your liver’s doing the tango with lipids while your gallbladder gets a front-row seat to the tragedy.
Also-emoji for gallstones: 💎😭
Stop eating butter. Start walking. Or just… accept your fate. We’re all just carbon-based machines with faulty firmware anyway.
James Steele
December 5, 2025 AT 12:58Let’s be real-fenofibrate is the pharmaceutical equivalent of giving a pyromaniac a matchbox and calling it ‘fire safety training.’
The PPAR-alpha pathway? Elegant. Beautiful. A masterpiece of molecular choreography. And yet-like all great art-it leaves a scorched earth behind. Cholesterol saturation in bile isn’t a side effect-it’s the crescendo.
And the fact that we’re still treating this like a ‘risk-benefit’ calculus instead of a systemic failure of drug surveillance? That’s the real tragedy. We optimize for LDL numbers while ignoring the visceral cost. We’ve turned medicine into a spreadsheet.
Meanwhile, the 5% who get stones? They’re not statistics. They’re the collateral damage of our obsession with biomarkers over biology.
Louise Girvan
December 6, 2025 AT 07:41EVERYONE KNOWS FENOFIBRATE CAUSES GALLSTONES-BUT THE PHARMA COMPANIES PAY DOCTORS TO STAY QUIET!!
YOU THINK THAT 2021 STUDY WAS ‘INDEPENDENT’? HA!!
THEY’RE ALSO HIDING THAT URSODIOL IS BANNED IN 17 COUNTRIES BECAUSE IT CAUSES LIVER FAILURE!!
YOUR DOCTOR ISN’T YOUR FRIEND-SHE’S A PAID SPokesperson!!
GET THE ULTRASOUND OR DIE!!
AND DON’T TRUST ‘DIET’-IT’S A DISTRACTION!!
THEY WANT YOU TO BLAME YOURSELF!!
THEY WANT YOU TO EAT LESS BUTTER!!
WHILE THEY MAKE BILLIONS!!
WAKE UP!!
soorya Raju
December 7, 2025 AT 21:11bro fenofibrate is just big pharma’s way of selling more surgeries 😭
in india we dont even use this drug much-too expensive and too many ppl get stones
my uncle took it for 2 years and ended up in hospital with jaundice
they said ‘its rare’ but rare dont feel like your insides are being chewed by a rat
why dont they test bile composition before prescribing? why not just give omega 3 and tell people to walk? simple stuff
also i think the FDA is bribed by swiss pharma companies lol
typo: cholecystectmy = cholecystectomy 😅
Dennis Jesuyon Balogun
December 8, 2025 AT 21:30Let me speak to the soul of this issue.
We treat the body like a machine to be tuned-not a living, breathing ecosystem.
Fenofibrate doesn’t ‘cause’ gallstones-it exposes a deeper imbalance. The liver is screaming. The gallbladder is holding its breath. And we give it more chemicals instead of listening.
This isn’t about drugs or diets. It’s about how we’ve lost the art of healing and replaced it with intervention.
If your bile is too rich in cholesterol, it’s not because of fenofibrate alone. It’s because your life is too rich in stress, sugar, and silence.
Walk. Breathe. Eat whole foods. Sleep. Connect. These aren’t ‘lifestyle hacks.’ They’re ancestral wisdom.
The stone isn’t the enemy. The disconnection is.
And if you’re reading this-you’re already one step closer to healing.
Grant Hurley
December 9, 2025 AT 11:46man i took fenofibrate for like 8 months and never felt a thing
but then i ate a whole pizza with extra cheese and suddenly felt like a grenade went off under my ribs
got an ultrasound-yep, 3 stones
doc said ‘you’re lucky it wasn’t worse’
so i stopped the drug, started walking 30 min a day, swapped out fried chicken for grilled salmon
2 months later-no more pain
no surgery
still take a statin
point is-you don’t need to be a hero
just be consistent
and listen to your body
it’s smarter than your doctor’s algorithm
Lucinda Bresnehan
December 9, 2025 AT 13:21Hey, I just wanted to say thank you for writing this. I’ve been on fenofibrate for 3 years and never knew about the gallstone risk. My mom had her gallbladder out when she was 52-she never told me why.
I went in for an ultrasound last week-turns out I had 4 silent stones. No pain, no clue.
My doctor switched me to ezetimibe and I’m already feeling better. No more bloating after dinner.
So if you’re on this med-please, please, get checked. Even if you feel fine. It’s not scary. It’s just a quick scan.
You’re not overreacting. You’re being smart.
And if you’re scared to talk to your doctor-I’ll help you draft an email. Just DM me. We got you.
Shannon Gabrielle
December 9, 2025 AT 18:25Oh wow. A 5% risk. How cute. Like getting struck by lightning while holding a cellphone in a thunderstorm. It’s rare. Until it’s you.
Meanwhile, the same people who prescribed this drug are now selling you ‘gallbladder-friendly’ supplements on Instagram.
They’re not your doctors. They’re your predators.
And yes-I know you’re eating kale now. Good for you. Too bad your bile is still a chemical waste dump.
Get the ultrasound. Or don’t. I’m sure your pain will be ‘just indigestion’ until it’s not.
Enjoy your ER visit.
ANN JACOBS
December 11, 2025 AT 10:50It is with profound gratitude and a deep sense of responsibility that I offer this reflection on the matter at hand.
The administration of fenofibrate, while statistically efficacious in the reduction of triglyceride levels and the augmentation of high-density lipoprotein concentrations, introduces a significant pathophysiological perturbation within the biliary system, precipitating cholesterol supersaturation and subsequent crystallization.
It is therefore not merely prudent, but ethically imperative, that patients undergoing such pharmacological intervention be subjected to proactive, longitudinal imaging surveillance, particularly those who present with predisposing factors such as advanced age, female sex, metabolic syndrome, or familial predisposition.
Moreover, the integration of dietary modification-emphasizing the reduction of saturated fats, the augmentation of dietary fiber, and the promotion of regular, low-intensity physical activity-constitutes a foundational pillar of preventive care.
One must not underestimate the cumulative impact of behavioral adherence. The data is unequivocal. The evidence is robust. The opportunity for intervention is now.
Let us not be passive recipients of pharmaceutical innovation. Let us be informed, vigilant, and proactive stewards of our own physiological integrity.
With sincere regard for your health and well-being,
Ann Jacobs, Ph.D., M.P.H.
Nnaemeka Kingsley
December 12, 2025 AT 02:09bro, my cousin took this drug and got stones
he was scared to tell anyone
but after surgery, he said: ‘i wish i just walked more and ate less fried food’
you dont need to be rich to be healthy
you just need to care
and listen to your body
it tells you things
if you stop and hear it
you dont need fancy tests
just eat clean, move, sleep
and talk to your doc
they dont know everything
but they can help if you ask
Kshitij Shah
December 12, 2025 AT 07:16So fenofibrate = gallstones. Cool.
Meanwhile in India, people get stones from eating too much ghee and not moving. Same outcome. Different villain.
Western medicine blames the pill. Eastern medicine blames the plate.
Both right.
But here’s the real twist: the pill was meant to fix the plate.
So who’s the real problem?
Maybe it’s not the drug.
Maybe it’s the idea that a pill can fix a lifestyle.
Just saying.
Also-my uncle took fenofibrate and lived to 87. No stones.
So maybe it’s not the drug.
Maybe it’s the person.
Or maybe it’s both.
Either way-walk more. Eat less junk. And stop blaming the medicine.