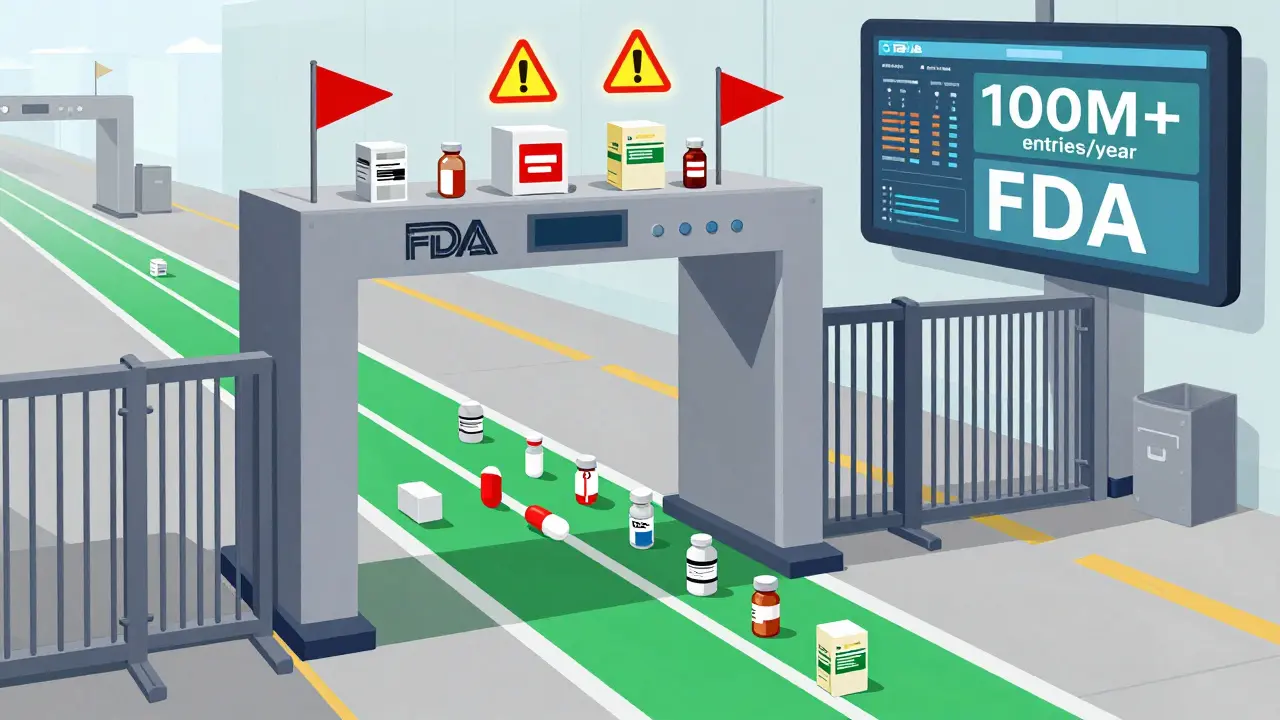
The U.S. doesn’t just open its borders to every drug shipment that arrives. Every pill, vial, and capsule entering the country - whether it’s from a giant pharmaceutical plant in India or a small lab in Germany - goes through a strict, high-tech screening system run by the FDA. This isn’t a casual check. It’s a full-scale operation designed to stop contaminated, fake, or illegal drugs from reaching patients. And since October 2023, there’s no more loophole for small packages. Even shipments under $800, once considered too minor to bother with, are now fully inspected.
How the FDA Knows What’s Coming In
Before any drug hits U.S. soil, the importer must file an electronic entry with the FDA through the Prior Notice System Interface (PNSI). This isn’t optional. It’s required by law. The system gets details like the product name, manufacturer, quantity, port of entry, and shipping route. About 98% of these entries are reviewed automatically using risk-based algorithms. These tools don’t guess - they analyze patterns. Has this company had violations before? Is the product from a facility with a history of non-compliance? Is the shipment labeled correctly? If something looks off, the system flags it.The Five-Step Inspection Process
Once flagged or randomly selected, a shipment enters a five-phase review process:- Entry Submission: The importer submits all required documents - commercial invoice, bill of lading, and an Affirmation of Compliance (A of C) - proving the product meets U.S. standards.
- Entry Review: FDA analysts scan the submission. Incomplete forms, mismatched codes, or past violations trigger a hold. About 15.7% of entries get flagged this way.
- Examination and Sampling: If the product is selected for physical inspection, FDA staff at the port check the packaging, verify labels match FDA requirements (21 CFR Part 201), and may take 1-3 samples for lab testing. This step catches mislabeled drugs, missing active ingredients, or contamination.
- Compliance Review: Lab results are reviewed against U.S. standards. Did the drug meet current good manufacturing practices (cGMP)? Is the manufacturer registered? Is the product approved? If not, it’s detained.
- Final Admissibility Decision: The FDA decides: admit, refuse, or require corrective action. In 2022, 14.3% of physically inspected drug shipments were detained. Of those, nearly 68% were permanently refused entry.
What Gets Detained - and Why
Drugs get held for a handful of reasons - and they’re not always obvious. The most common issues:- Unapproved drugs: Products sold without FDA approval, often generic versions from overseas that never completed the application process.
- Improper labeling: Missing lot numbers, incorrect dosage instructions, or false claims like “FDA-approved” when they’re not.
- Contaminated ingredients: The 2022 valsartan recall was a wake-up call - contaminated active pharmaceutical ingredients (APIs) from India slipped through because they weren’t targeted.
- Unregistered facilities: If the factory isn’t registered with the FDA, the entire shipment is blocked, no matter how good the product looks.
- Counterfeit packaging: Fake pills made to look like brand-name drugs - often containing nothing, or worse, toxic substances.

The Fast Track: The Secure Supply Chain Pilot Program
Not all importers face the same delays. The FDA runs a program called the Secure Supply Chain Pilot Program (SSCPP), launched in 2019. It’s designed for companies with a flawless compliance record. If you’ve passed three straight years of inspections with zero violations, you can apply. Once accepted, you can designate up to five products for fast-track clearance.Companies like Johnson & Johnson use it. Their clearance time dropped from 7-10 days to under 48 hours. That’s a game-changer for just-in-time manufacturing. But here’s the catch: only 27 manufacturers are in the program as of late 2023. It’s not easy to get in. Smaller companies, especially generic drug makers, often can’t meet the bar. And even if they do, they’re still subject to random checks.
Where the System Falls Short
The FDA doesn’t have enough staff to inspect every shipment. With over 100 million drug entries annually, they physically examine only about 1.2% of them. That means the system relies heavily on risk targeting - and sometimes it misses things.In 2022, the Government Accountability Office found that only 4 of the 17 key performance metrics required by law had been fully implemented. That’s a red flag. The system tracks delays and detention rates, but it doesn’t reliably measure how many fake or dangerous drugs it actually stops. The Partnership for Safe Medicines estimates $4.3 billion in counterfeit drugs entered the U.S. in 2022 - mostly before the de minimis exemption was removed.
Another problem: inconsistency. At the Port of Los Angeles, only 5.2% of shipments were detained. At Miami, it was 18.7%. Why? Different staffing, different review teams, different interpretation of rules. Customs brokers report unpredictable delays - sometimes 2 days, sometimes 2 weeks - even for compliant shipments.
Who’s Affected - and How
The rules hit different groups in different ways.- Large pharma companies: They’ve built compliance teams. Many use FDA’s electronic systems daily. They benefit from the SSCPP and have direct contacts at ports to speed things up.
- Generic drug makers: Many face high detention rates - up to 37% for APIs from certain Indian facilities - even when their products are safe. The system doesn’t always distinguish between a risky facility and a compliant one.
- Biotech startups: Researchers importing biological samples for trials now face delays of 3-5 days and extra costs of $285-$420 per shipment. That slows down critical research.
- Small pharmacies and online sellers: Many don’t understand the rules. A single mislabeled box can trigger an Import Alert, which blocks all future shipments from that company - even if the error was minor.

What Importers Must Do Right
If you’re shipping drugs into the U.S., here’s what you need to get right:- Register your facility: Every manufacturer, repackager, or lab must be registered with the FDA. No exceptions.
- List your products: All drugs must be listed in the FDA’s Drug Listing System.
- Use correct codes: 28% of delays come from wrong product codes. Double-check the Harmonized System (HS) code.
- Match labels to FDA rules: No claims like “cures cancer” or “FDA-approved” unless it’s true. Include lot numbers, expiration dates, and manufacturer info.
- Keep records for 3 years: FDA can audit you anytime. Missing paperwork = detention.
Many importers hire customs brokers - but even they make mistakes. The best advice? Build a relationship with the FDA reviewer at your port. Companies that do report 22-35% faster clearance times.
What’s Changing in 2024
The FDA is upgrading its system. By mid-2024, the SSCPP will expand to 50 companies - including contract manufacturers. AI tools are being tested to improve risk targeting by 25%. A blockchain pilot will track drug movement from factory to pharmacy. And the FDA is working with international regulators through PIC/S to align standards.But the biggest change? The end of the de minimis exemption. Now, every shipment - no matter how small - is reviewed. That means 350,000 more entries per year for FDA to process. It’s a big burden, but it’s meant to close the door on the flood of fake pills and pill presses that used to slip through.
Final Reality Check
The FDA’s import system isn’t perfect. It’s underfunded, uneven, and sometimes slow. But it’s also the most advanced drug safety net in the world. The U.S. imports 88% of its active ingredients and 42.7% of its total drug supply. Without this system, the risk of tainted or fake drugs reaching patients would be far higher.For the average person, the system works quietly in the background. You never see it. But if you take a prescription pill, a vitamin, or even an over-the-counter pain reliever - it passed through this system. And that’s not a guarantee of safety. But it’s the best one we have.
Does the FDA inspect every drug shipment entering the U.S.?
No, but every shipment is reviewed electronically. Only about 1.2% of the 100+ million annual drug entries get a physical inspection. The FDA uses automated risk tools to target high-risk shipments - like those from past-violating facilities, unlabeled products, or shipments flagged by international partners. Since October 2023, even small shipments under $800 are included in this review.
What happens if a drug shipment is detained by the FDA?
If detained, the shipment is held at the port until the importer provides corrective action or proof of compliance. Options include re-labeling, destroying the product, or exporting it back. If the issue isn’t fixed within a set time, the FDA issues a refusal of admission. Repeated violations can lead to an Import Alert, which automatically detains all future shipments from that company.
Can I import prescription drugs from other countries for personal use?
Technically, importing prescription drugs for personal use is against FDA rules. But the agency often allows it if the drug is for a serious condition, not commercially available in the U.S., and for no more than a 90-day supply. However, there’s no guarantee - the FDA can still seize the shipment. Importing drugs from online pharmacies outside the U.S. is risky - many are counterfeit or unregulated.
How can I check if a drug manufacturer is FDA-registered?
Go to the FDA’s Drug Registration and Listing System (DRLS) database. You can search by company name, facility location, or product. If a facility isn’t listed, the drugs it makes are not legally allowed to be imported into the U.S. Always verify this before ordering from overseas suppliers.
Why do some shipments get cleared quickly while others are held for weeks?
It depends on risk level, documentation accuracy, and port workload. High-risk products (e.g., from flagged facilities, unregistered manufacturers, or with labeling issues) get held longer. Clean, complete submissions from trusted importers under the SSCPP clear in 24-48 hours. Inconsistent staffing and manual reviews at different ports also cause delays. Building a relationship with your port’s FDA reviewer can reduce wait times significantly.

Helen Leite
January 24, 2026 AT 03:39Sushrita Chakraborty
January 25, 2026 AT 11:51