Ipratropium Bromide Dosage Calculator
Determine Your Recommended Dose
Quick Takeaways
- Use a ipratropium bromide inhaler twice daily for COPD and up to four times for acute asthma symptoms.
- Shake the inhaler, exhale fully, then inhale slowly while pressing the dose.
- Space out doses at least 6 hours apart; never exceed the recommended total daily dose.
- Combine with a short‑acting beta‑agonist (e.g., albuterol) for faster relief.
- Watch for dry mouth, cough, or throat irritation - rinse your mouth after each use.
What is Ipratropium Bromide Inhaler is a handheld device that delivers the bronchodilator ipratropium bromide directly to the airways?
Ipratropium bromide belongs to the short‑acting muscarinic antagonist (SAMA) class. It blocks acetylcholine receptors in the bronchial smooth muscle, preventing the muscle from tightening. The result is wider airways and easier breathing.
The inhaler comes pre‑filled with 78 µg per puff (commonly sold as 2 µg per actuation in a metered‑dose inhaler, MDIs) and is designed for oral inhalation, not nebulization.
How It Works in the Lungs
When you press the canister, a fine mist of ipratropium particles is released. These particles settle on the bronchial lining within seconds. By competitively inhibiting the M3 muscarinic receptors, the drug stops the cascade that leads to smooth‑muscle contraction.
Because it works locally, systemic side effects are rare compared with oral anticholinergics. The onset of action is about 5‑15 minutes, and the effect lasts 4‑6 hours.
When to Use It: COPD vs. Asthma
COPD is a progressive lung disease characterized by chronic airflow limitation. Ipratropium is a mainstay for maintenance therapy, especially for patients who experience frequent exacerbations.
In Asthma is a reversible airway disease driven by inflammation and hyper‑responsiveness, ipratropium is usually added as a rescue add‑on when a short‑acting beta‑agonist alone isn’t enough.
Other situations include:
- Bronchospasm during acute upper‑respiratory infections.
- Pre‑exercise prophylaxis for patients with exercise‑induced bronchoconstriction who can’t tolerate beta‑agonists.
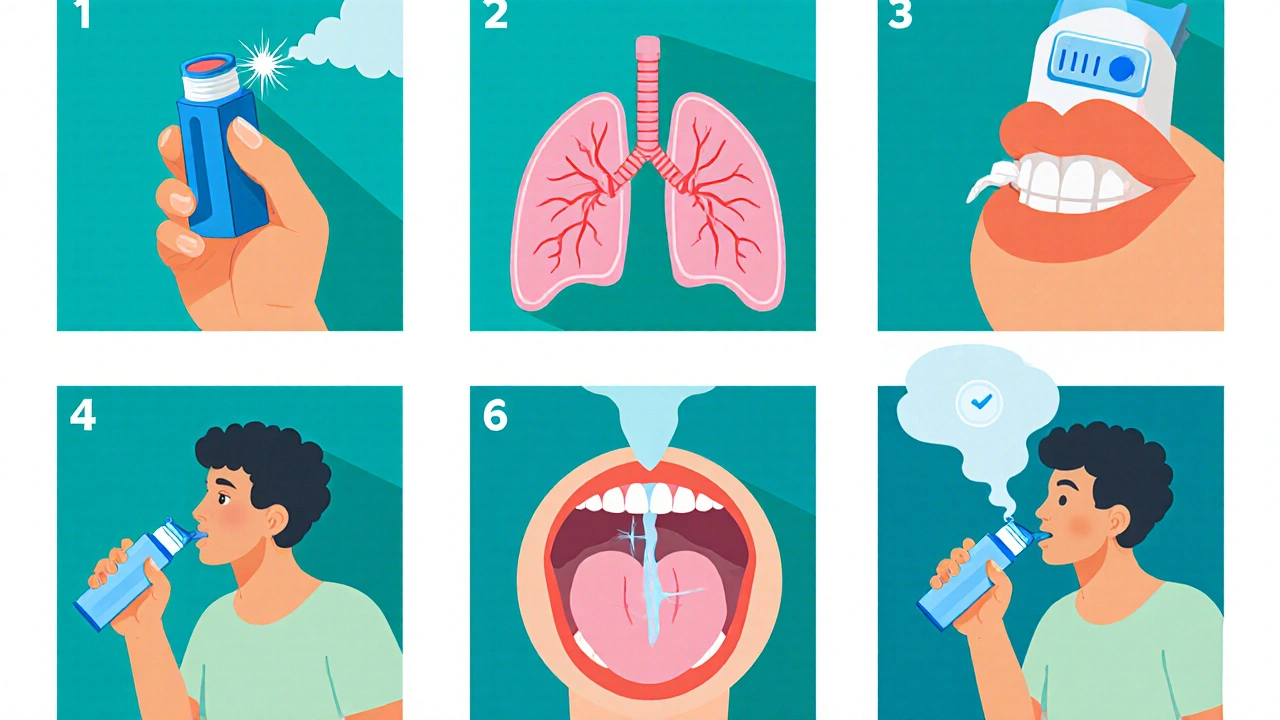
Proper Inhaler Technique - Step by Step
- Remove the cap and check the mouthpiece - it should be clean and free of debris.
- Shake the inhaler vigorously for at least 5 seconds.
- Exhale fully, emptying your lungs but do NOT exhale into the mouthpiece.
- Place the mouthpiece between your teeth, seal your lips around it, and keep your tongue flat.
- Press down on the canister once while breathing in slowly and deeply through the mouth.
- Hold your breath for about 10 seconds, then exhale slowly.
- If a second puff is prescribed, wait at least 30 seconds before repeating the steps.
- Replace the cap securely after use.
Using a Spacer Device is an optional chamber that helps slow the particle velocity, improving deposition in the lungs can make the technique easier for children or people with limited hand‑lung coordination.
Dosage Guidelines
| Condition | Adult Dose | Frequency | Maximum Daily Dose | Special Note |
|---|---|---|---|---|
| COPD (maintenance) | 2 puffs (78 µg per puff) | Twice daily (morning & evening) | 4 puffs (312 µg) | Can be combined with a long‑acting beta‑agonist. |
| Acute asthma (rescue) | 2 puffs | Every 4-6 hours as needed | 8 puffs (624 µg) per 24 h | Use alongside albuterol for faster symptom relief. |
| Pediatric (age 6‑12) | 1 puff | Twice daily | 2 puffs (156 µg) per day | Ensure child can coordinate inhalation; use a spacer. |
Never exceed the listed maximum daily dose. Over‑use can lead to paradoxical bronchospasm or increased anticholinergic side effects.
Common Mistakes and How to Avoid Them
- Not shaking the inhaler: The medication can settle, delivering a weaker dose.
- Breathing in too fast: Fast inhalation pushes particles to the mouth instead of the lungs.
- Exhaling into the mouthpiece: Moisture can clog the nozzle.
- Skipping the spacer for children: A spacer improves deposition and reduces oral irritation.
- Using past‑date inhalers: Check the expiration; potency drops after the listed date.
Managing Side Effects
Most users experience mild, local effects. Common complaints include dry mouth, throat irritation, and a hoarse voice. Simple tricks help:
- Rinse your mouth with water after each dose - this reduces residue.
- Use a humidifier at night if you have chronic dry throat.
- Keep the inhaler upright when not in use to prevent leakage.
Rare systemic effects (e.g., urinary retention, blurred vision) usually signal over‑use or an interaction with other anticholinergic drugs. If they appear, contact your healthcare provider promptly.
Monitoring Your Progress
A Peak Flow Meter is a handheld device that measures the highest speed of exhaled air, giving a quick snapshot of airway openness can help you track how well ipratropium is working. Record your peak flow every morning and evening; a consistent decline may signal the need for a dose adjustment.
Regular follow‑up appointments-ideally every 3-6 months-allow your clinician to review technique, dosage, and overall lung function.
Frequently Asked Questions
Can I use ipratropium with my rescue inhaler?
Yes. It’s common to pair ipratropium with a short‑acting beta‑agonist like albuterol. The two agents work via different pathways, giving faster and more complete relief.
Is it safe to use ipratropium during pregnancy?
Current data show no clear teratogenic risk, but you should always discuss any medication with your obstetrician. The lowest effective dose is recommended.
What should I do if I miss a dose?
Take the missed dose as soon as you remember, unless it’s within 1 hour of the next scheduled dose. In that case, skip the missed one and resume your regular schedule. Never double up.
Can children under 6 use ipratropium?
The inhaler is not approved for children younger than 6 years. For younger kids, a nebulized formulation under medical supervision is preferred.
Why does my throat feel dry after each puff?
Ipratropium’s anticholinergic action reduces secretions, leading to dryness. Rinsing your mouth and staying hydrated usually eases the symptom.
Proper use of an ipratropium bromide inhaler can make a big difference in daily breathing comfort. Stick to the technique, respect the dosage limits, and keep an eye on side effects. When in doubt, your pharmacist or prescribing clinician is the best person to guide you.


Wesley Humble
October 20, 2025 AT 15:05First and foremost, the inhaler technique delineated in the article warrants meticulous adherence, as any deviation can attenuate drug deposition in the lower airways. The protocol of shaking the canister for a full five seconds ensures homogenous suspension of the medication, thereby preventing sub‑therapeutic dosing. Exhaling completely before insertion of the mouthpiece eliminates residual air that might otherwise dilute the aerosol plume. The recommendation to inhale slowly while simultaneously actuating the device maximizes particle penetration into the bronchioles rather than depositing in the oropharynx. Holding one's breath for approximately ten seconds allows the bronchodilator to diffuse across the mucosal surface, facilitating prompt bronchodilation. Moreover, the spacing of doses by at least six hours mitigates the risk of cumulative anticholinergic side effects, especially dry mouth and throat irritation. Patients should be counseled to rinse their mouths after each puff to reduce the propensity for oral candidiasis – a point often overlooked in primary care settings. The inclusion of a spacer, particularly for pediatric users or those with limited hand‑lung coordination, has been substantiated by numerous randomized trials to improve lung‑dose efficiency. It is equally imperative to verify the expiration date; expired propellants may deliver inconsistent dose volumes. In the context of COPD maintenance, the twice‑daily regimen of two puffs aligns with current GOLD guidelines, whereas acute asthma exacerbations may necessitate up to four puffs per day, not exceeding the stipulated maximum. Combining ipratropium with a short‑acting beta‑agonist such as albuterol confers synergistic bronchodilation via complementary pharmacologic pathways. Patients should monitor peak flow values routinely; a sustained decline may indicate suboptimal inhaler technique or disease progression. Should systemic anticholinergic manifestations such as urinary retention surface, immediate medical evaluation is advised. Finally, regular follow‑up appointments every three to six months enable clinicians to reassess technique, dosage, and overall disease control. Adherence to these comprehensive measures ultimately translates to enhanced quality of life for individuals grappling with obstructive airway disease 😊
barnabas jacob
October 24, 2025 AT 07:58Yo, u think u’re a PhD on inhaler tech, but u missed the fact that “actuation” ain’t just a buzzword – it’s a c**k‑up if you don’t coordinate timing. The whole “shake for five seconds” thing is peripheral, real compliance hinges on patient education, not just fancy prose. Also, u didn’t even mention the role of propellant temperature in aerosol particle size – that’s a major oversight. Stop actin’ like a textbook and give folks some real‑world tips.
Vijaypal Yadav
October 27, 2025 AT 23:51In terms of dosage, the standard adult regimen for COPD is two puffs twice daily, which translates to 156 µg per day. For acute asthma episodes, the ceiling of eight puffs in a 24‑hour period provides up to 624 µg, staying within safety margins. Pediatric patients aged six to twelve should receive a single puff twice daily, totaling 156 µg daily, and a spacer is highly recommended to ensure optimal deposition.
Ron Lanham
October 31, 2025 AT 16:45It is incumbent upon every healthcare professional to recognize that prescribing an ipratropium bromer inhaler without thorough instruction is tantamount to negligence, because proper technique is the linchpin of therapeutic efficacy. When patients are left to fumble through ambiguous directions, they not only squander medication but also endure unnecessary dyspnea, which could have been averted with clear guidance. We must therefore champion patient education as an ethical imperative, not a perfunctory afterthought. The responsibility extends beyond the clinic walls; pharmacists, nurses, and even caregivers share in the duty to reinforce the step‑by‑step protocol, ensuring that each inhalation is executed with precision. Moreover, the integration of a spacer should be advocated for any individual who struggles with hand‑lung coordination, as the device markedly improves drug delivery to the lower respiratory tract. This is not merely a convenience but a clinical necessity, especially for the pediatric and geriatric populations who are most vulnerable to suboptimal dosing. By upholding these standards, we safeguard against avoidable exacerbations and reduce the burden on emergency services, thereby aligning with the broader public health goal of minimizing healthcare costs. Let us, therefore, make it a point to revisit inhaler technique at each follow‑up visit, treat it with the gravitas it deserves, and empower patients to become competent stewards of their own respiratory health.
Deja Scott
November 4, 2025 AT 09:38I appreciate the clear, step‑by‑step layout of the inhaler instructions.
Natalie Morgan
November 8, 2025 AT 02:31Great point about education-regular technique checks can truly cut down on avoidable flare‑ups.
Mahesh Upadhyay
November 11, 2025 AT 19:25Spacer devices are a game‑changer for anyone struggling with coordination.
Rajesh Myadam
November 15, 2025 AT 12:18I’ve seen patients who were skeptical at first, but after a few weeks with a spacer their peak flow numbers improved noticeably, which made them more confident in using the inhaler correctly.
Andrew Hernandez
November 19, 2025 AT 05:11From a cultural perspective, it’s interesting how inhaler etiquette varies globally, yet the core principle of proper technique remains universal.
Alex Pegg
November 22, 2025 AT 22:05Some users obsess over every nuance of inhaler usage, but in reality, as long as the dose is taken, the minor variations in breath hold or shake duration don’t dramatically alter outcomes.
laura wood
November 26, 2025 AT 14:58I understand how frustrating it can be to manage a chronic condition, and a solid inhaler routine can provide a sense of control amidst the uncertainty.
Kate McKay
November 30, 2025 AT 07:51Keep tracking your peak flow each morning and evening; noticing trends will help you and your provider fine‑tune the regimen before symptoms flare.
Demetri Huyler
December 4, 2025 AT 00:45While you downplay the importance of precision, the evidence from American thoracic societies underscores that meticulous technique directly correlates with reduced hospitalization rates, a fact your casual attitude overlooks.
JessicaAnn Sutton
December 7, 2025 AT 17:38The article’s dosage table is accurate, yet it omits the critical advisory that patients with renal impairment may require dose adjustments to avoid systemic accumulation.