Methotrexate-NSAID Interaction Risk Calculator
This tool estimates the risk of methotrexate toxicity when taking NSAIDs based on your kidney function and NSAID type. Always consult your healthcare provider before changing medications.
Why Mixing Methotrexate and NSAIDs Can Be Dangerous
Take methotrexate for rheumatoid arthritis? You’ve probably been told to avoid NSAIDs like ibuprofen or naproxen. But why? It’s not just a vague warning-it’s a real, measurable risk that can land you in the hospital. Methotrexate is cleared by your kidneys. NSAIDs slow down kidney function. Together, they can cause methotrexate to build up to toxic levels, leading to kidney injury, low blood cell counts, and even death.
Here’s the hard truth: in 2022, the FDA reported three deaths linked to this exact combination in just four years. Most of these cases happened because no one checked kidney function before or after starting the NSAID. It’s not rare. Around 1.3 million Americans take low-dose methotrexate for autoimmune diseases. A huge number of them also take NSAIDs for joint pain. That’s a ticking time bomb if you’re not monitoring it.
How Methotrexate Works-and Why Kidneys Matter
Methotrexate isn’t just a single drug. It’s used at low doses (5-25 mg weekly) for rheumatoid arthritis, and at high doses (over 150 mg per day) for cancer. Either way, your kidneys are the main way it leaves your body. About 80% of it gets filtered out through urine. At low doses, it’s mostly eliminated unchanged. At high doses, the system gets overloaded, and clearance slows down even more.
That’s why timing and kidney health are everything. Methotrexate peaks in your blood 45 minutes to 6 hours after taking it. If your kidneys aren’t working well-or if something else is slowing them down-methotrexate sticks around. And when it does, it starts damaging your bone marrow, liver, and gut lining. Symptoms? Fatigue, mouth sores, nausea, low white blood cell counts. In severe cases, it’s life-threatening.
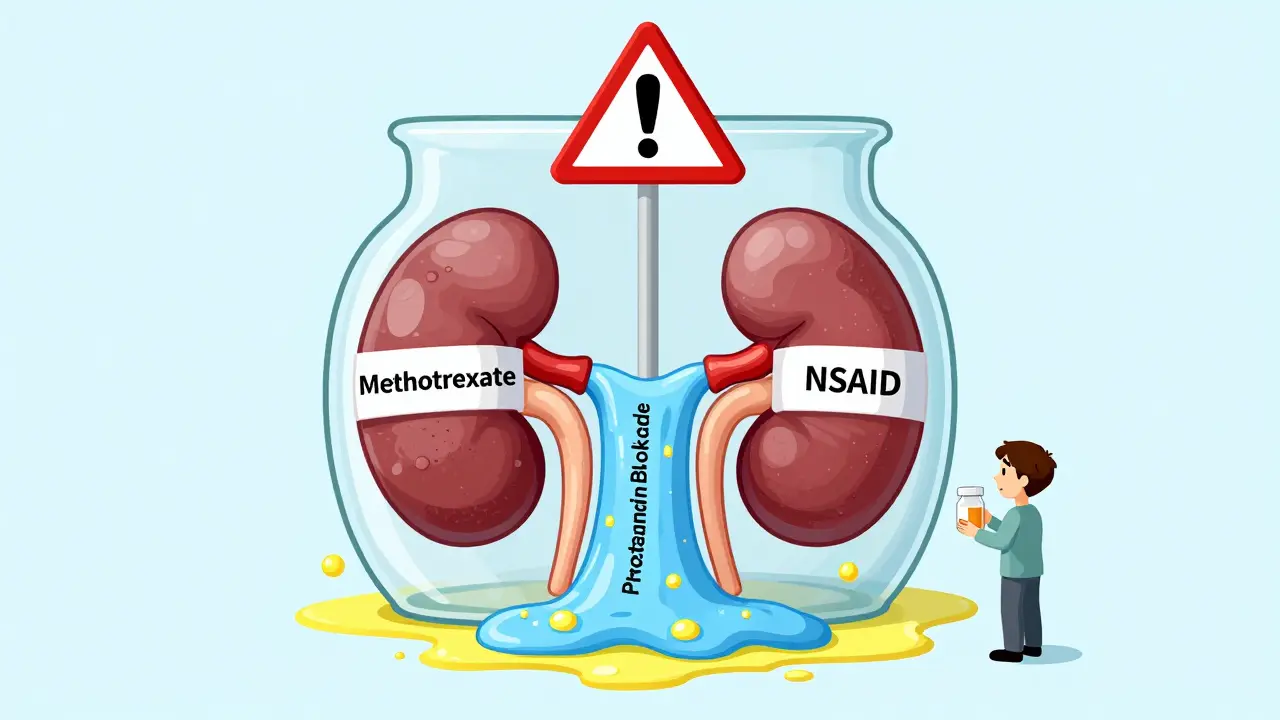
How NSAIDs Interfere-It’s Not Just One Thing
NSAIDs don’t just cause stomach upset. They block prostaglandins, chemicals your kidneys need to keep blood flowing properly. Less blood flow = less filtering. Studies show NSAIDs can reduce kidney blood flow by 15-20%. That’s enough to cut methotrexate clearance by 25-40%.
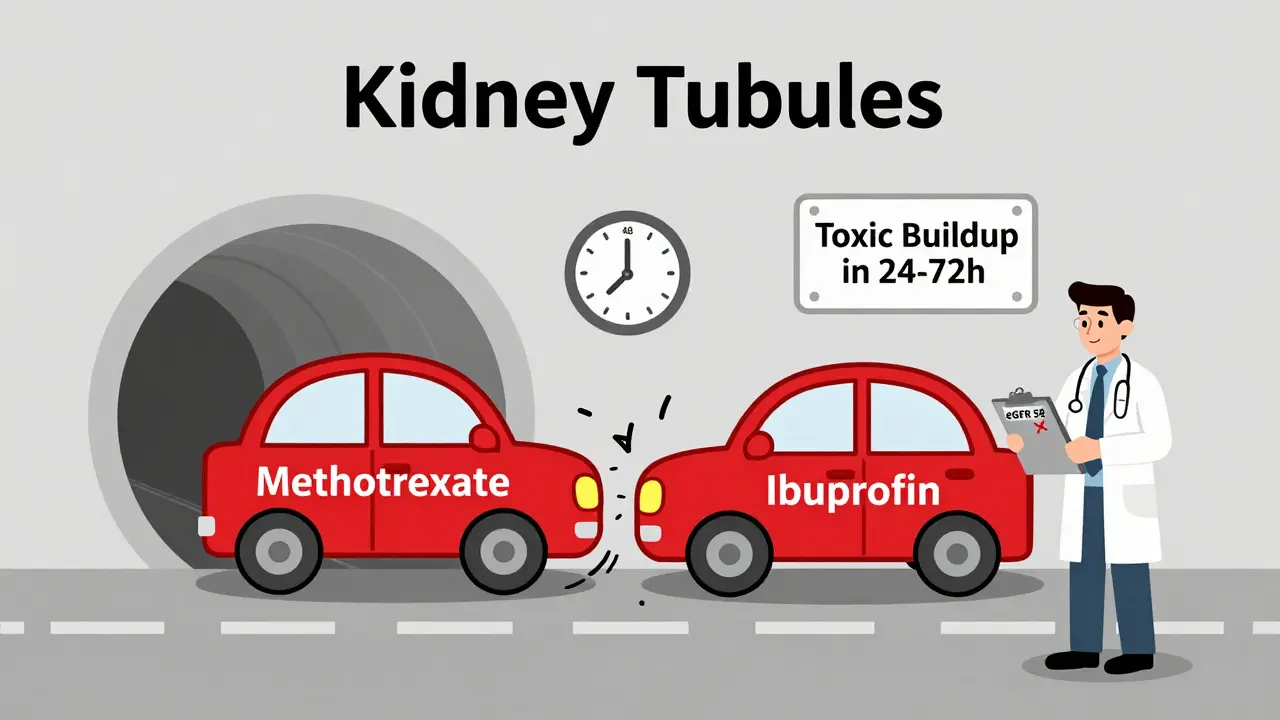
But there’s more. NSAIDs also compete with methotrexate for the same transporters in the kidney tubules. Think of it like two cars trying to get through a narrow tunnel at the same time. One gets stuck. Methotrexate gets stuck. This is called competitive inhibition-and it’s why even small doses of NSAIDs can push methotrexate levels up by 25-50%.
And then there’s protein binding. Methotrexate normally sticks to proteins in your blood, which keeps it from being too active. NSAIDs can knock it loose. That means more free, active methotrexate floating around-up to 30% more-increasing toxicity even if total levels don’t look scary.
Not All NSAIDs Are Created Equal
If you must use an NSAID, not all are the same risk. Ketorolac is the worst offender. It’s potent, short-acting, and causes the biggest drop in kidney blood flow. Studies show it can spike methotrexate levels by up to 50%. That’s why it’s banned in many hospitals for patients on methotrexate.
Ibuprofen? Moderate risk. It raises methotrexate levels by about 25-30%. Naproxen? Similar. Diclofenac? Also risky.
Celecoxib is the safest option among NSAIDs. Because it only blocks COX-2 (not COX-1), it’s gentler on kidney blood flow. Studies show it increases methotrexate levels by only 10-15%. That’s still not zero-but it’s the best choice if you absolutely need an NSAID.
Here’s a quick comparison:
| NSAID | Estimated Increase in Methotrexate Levels | Risk Level |
|---|---|---|
| Ketorolac | 40-50% | Extreme |
| Ibuprofen, Naproxen, Diclofenac | 25-35% | High |
| Celecoxib | 10-15% | Moderate |
| Acetaminophen (Tylenol) | 0% | Safe |
High-Dose vs. Low-Dose Methotrexate: Big Difference in Risk
This interaction is way more dangerous with high-dose methotrexate-like what’s used for cancer. In those cases, adding an NSAID increases the risk of severe toxicity by nearly five times. That’s why oncology guidelines say: don’t use NSAIDs at all during high-dose therapy unless there’s no other option-and even then, you must check methotrexate levels at 24, 48, and 72 hours after the infusion.
For low-dose methotrexate (the kind most RA patients take), the picture is murkier. One big 2019 study of over 4,000 RA patients found no major increase in side effects when NSAIDs were used with normal kidney function. But here’s the catch: that study only looked at people with healthy kidneys. When kidney function was already low (eGFR under 60), the risk jumped 3.5-fold. Another study found that 78% of serious cases happened in people who hadn’t had a kidney test in the past 30 days.
So if your eGFR is above 60 and you’re young and otherwise healthy, the risk might be low-but it’s not zero. If you’re over 65, have diabetes, high blood pressure, or any kidney trouble? Avoid NSAIDs completely.
What Doctors and Pharmacists Should Do
Guidelines from the American College of Rheumatology and EULAR are clear:
- Don’t use NSAIDs if your eGFR is below 60 mL/min/1.73m².
- If you must use one, pick celecoxib and use the lowest dose for the shortest time.
- Space out your doses-take methotrexate and NSAIDs at least 12 hours apart.
- Test your creatinine and complete blood count 48-72 hours after starting the NSAID.
Pharmacists are the frontline here. A 2023 study showed that when pharmacists actively screened for this interaction in Medicare patients, the number of dangerous combinations dropped by 63%. That’s because they catch it before the prescription is filled. They remind doctors. They educate patients.
And patients? They need to know. On CreakyJoints, 62% of people said they were never warned about this interaction. One Reddit user ended up with a white blood cell count of 1.8 (normal is 4-11) after taking naproxen without a kidney test. He needed leucovorin-a rescue drug-to survive.
What You Can Do as a Patient
If you’re on methotrexate:
- Ask your doctor: “What’s my eGFR? Is it above 60?”
- Never start an NSAID without checking your kidney function first.
- Get blood tests 48-72 hours after starting any new NSAID.
- Report fatigue, mouth sores, or nausea right away-don’t wait.
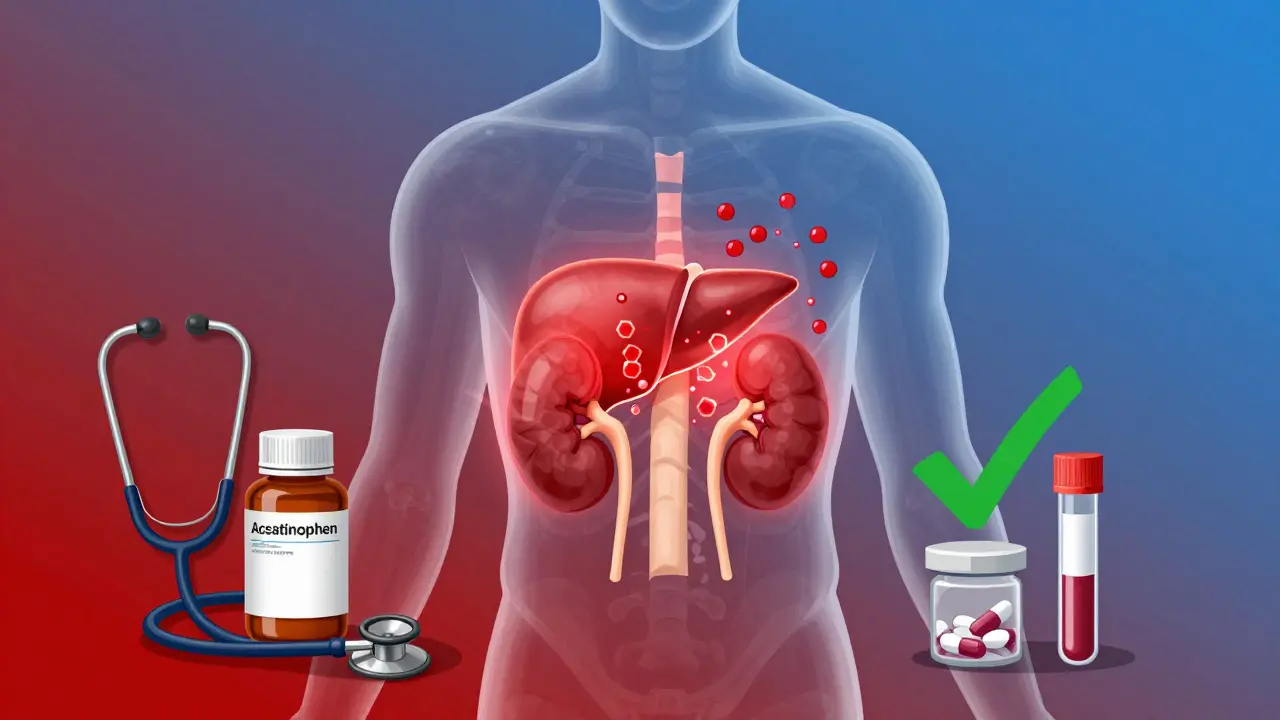
- Ask about alternatives: acetaminophen (up to 3,000 mg/day), physical therapy, or adjusting your DMARDs to reduce inflammation.
Some people manage this combo for years with no issues. But they all have one thing in common: they get tested regularly. That’s the difference between safety and disaster.
What’s Next? Genetic Testing and Real-Time Monitoring
Scientists are finding that not everyone is equally at risk. A gene called SLC19A1 affects how your kidneys take up methotrexate. About 15% of Caucasians have a variant that makes them absorb more methotrexate-especially when NSAIDs are around. These people can see methotrexate levels jump 40% higher than others.
Right now, genetic testing isn’t routine. But it’s coming. In phase 3 trials right now are handheld devices that can measure methotrexate levels in your blood within minutes. Imagine being able to check your levels right after taking an NSAID-before you even feel sick. That could change everything.
Until then, the rules are simple: know your kidney numbers. Test before you start an NSAID. Test again after. Don’t guess. Don’t assume. This interaction kills. But it’s preventable.
Can I take ibuprofen with methotrexate if I have normal kidney function?
It’s possible, but not without risk. Even with normal kidneys, ibuprofen can raise methotrexate levels by 25-30%. Use the lowest dose for the shortest time-no more than 3-5 days. Always get a creatinine and CBC test 48-72 hours after starting it. If you’re over 65, have high blood pressure, or diabetes, avoid it entirely.
What’s the safest painkiller to take with methotrexate?
Acetaminophen (Tylenol) is the safest option. It doesn’t affect kidney blood flow or methotrexate clearance. Stick to 3,000 mg per day max. For long-term pain, focus on controlling the underlying inflammation with your DMARDs or biologics instead of masking symptoms with NSAIDs.
How long does it take for methotrexate levels to rise after taking an NSAID?
The rise can happen within 24-48 hours. That’s why blood tests are recommended at 48-72 hours after starting the NSAID. Symptoms like fatigue or mouth sores may appear later, but the kidney damage and drug buildup happen fast. Waiting for symptoms is too late.
Can I take NSAIDs occasionally, like once a month?
Even occasional use can be risky if your kidney function is borderline. Each exposure adds up. The 2023 Institute for Safe Medication Practices lists this combination as a top 10 high-alert interaction because even infrequent use has caused serious harm. Better to avoid NSAIDs completely unless you’re under strict monitoring.
What should I do if I already took an NSAID with methotrexate?
Stop the NSAID immediately. Call your doctor or pharmacist. Ask for a creatinine and CBC test within the next 24-48 hours. Watch for signs of toxicity: extreme tiredness, fever, mouth ulcers, bruising, or dark urine. If you feel worse, go to the ER. Leucovorin can reverse toxicity if given early.
Bottom Line: Don’t Guess. Test.
Methotrexate and NSAIDs don’t mix safely without oversight. The risk isn’t theoretical-it’s documented in deaths, hospitalizations, and lab results. The difference between safety and disaster is a simple blood test. If you’re on methotrexate, your kidneys are your most important organ right now. Protect them. Ask for your eGFR. Test before you take an NSAID. And if your doctor says it’s fine without checking-get a second opinion. Your life isn’t worth the risk of a bad guess.