Rebound Congestion Recovery Calculator
Recovery Assessment
Recovery Timeline
Enter your usage details above to see your personalized recovery timeline.
Ever used a nasal decongestant spray for a few days, only to find your nose feels more blocked than before? You’re not alone. What feels like a cold that won’t quit might actually be something called rhinitis medicamentosa - a condition caused by overusing nasal decongestant sprays. It’s not a bug or allergy. It’s a side effect you didn’t see coming. And it’s more common than you think.
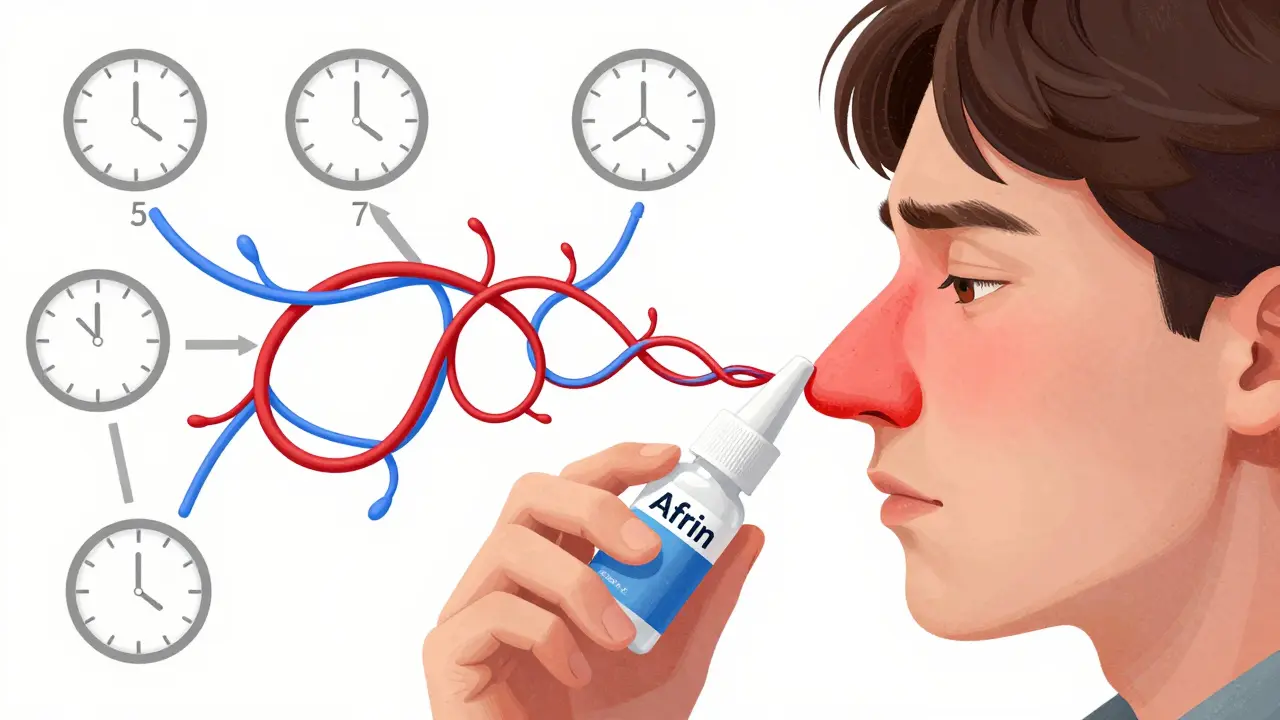
How Your Nasal Spray Is Making Things Worse
Nasal decongestant sprays like Afrin, Neo-Synephrine, and Vicks Sinex work fast. They shrink swollen blood vessels in your nose, giving you instant relief. But here’s the catch: your body gets used to them. After three to four days, the effect wears off - and your nasal passages swell even more than before. This is called rebound congestion. The spray that helped you now keeps you hooked. The active ingredients - oxymetazoline, phenylephrine, or xylometazoline - cause blood vessels to constrict. When they wear off, the vessels dilate too much, creating a cycle. You spray again. It helps. Then it fails. You spray more. And the cycle gets worse. According to the National Center for Biotechnology Information, this isn’t rare. About 10% of people who use these sprays past the recommended time develop it. In the U.S. alone, half a million cases are diagnosed every year.What It Feels Like
If you’ve been using a nasal spray for more than a week, here’s what you might be experiencing:- Nasal stuffiness that returns as soon as the spray wears off
- No runny nose - just constant blockage
- Needing to spray more often - every 4 hours, then every 2
- Difficulty breathing through your nose, even at night
- Dry mouth, snoring, or mouth breathing because your nose won’t stay open
The Only Way Out: Stop the Spray
The good news? This condition is reversible. The bad news? You have to quit the spray - completely. There’s no shortcut. Stopping is the only proven way to reset your nasal passages. But quitting cold turkey can be rough. For the first few days, congestion often gets worse. That’s normal. It’s your body adjusting. The key is to stick with it. Most people start feeling better within 7 to 14 days. But without a plan, many give up and go back to the spray.How to Quit Without Losing Your Mind
There are smart ways to stop - and ways that make it harder. Here’s what works:- One nostril at a time: Stop using the spray in one side first. Wait until it clears up (usually 3-5 days), then stop on the other side. This method, recommended by Mayo Clinic, helps you keep at least one airway open during withdrawal. A WebMD survey found 63% of people who used this approach said their symptoms were manageable.
- Don’t stop both at once: Quitting both sides simultaneously often leads to severe discomfort. Many people relapse within days because they can’t breathe.
- Use saline rinses: Flush your nose with a saltwater solution (neti pot or squeeze bottle) 2-3 times a day. It reduces swelling, clears mucus, and soothes irritated tissue. A 2022 review showed 60% of patients got relief from saline alone.

What to Use Instead
While your nose heals, you need alternatives. Here’s what doctors recommend:- Intranasal corticosteroids: Flonase (fluticasone) and Nasonex (mometasone) are the gold standard. They reduce inflammation without causing rebound. Studies show 68-75% of users see major improvement within 2-4 weeks. Use them twice daily at first, then once daily as symptoms improve.
- Oral steroids (short-term): For severe cases, a 5-day course of prednisone (0.5 mg per kg of body weight) can break the cycle fast. One 2021 study found 82% of patients improved significantly.
- Capsaicin spray: Made from chili pepper extract, this is used in Europe and shows promise. It desensitizes nerve endings in the nose. In European trials, it helped 55% of users - less than corticosteroids, but still useful for some.
What to Avoid
Not all congestion remedies are safe when you’re recovering:- Oral decongestants: Pseudoephedrine and phenylephrine can raise blood pressure. One study found 1 in 7 hypertensive patients had dangerous spikes when using them.
- Antihistamines: These dry out your nose and can make congestion feel worse if you don’t have allergies.
- More nasal sprays: Even if it’s a different brand, if it’s a decongestant, it’ll restart the cycle.
What Recovery Looks Like
Here’s what a typical 14-day recovery looks like:- Days 1-3: Worst congestion. Use saline rinses every 2 hours. Start Flonase twice daily.
- Days 4-7: Congestion eases slightly. You might feel pressure or headaches. Keep rinsing and using corticosteroid spray.
- Days 8-14: Breathing improves. You can sleep through the night. Switch Flonase to once daily.

Why Most People Fail
Relapse is common. Cleveland Clinic data shows that 22% of patients go back to nasal sprays if they don’t get counseling. Only 7% relapse with proper guidance. Why? Because the first few days are brutal. Your brain screams for relief. You think, “Just one spray to get through the night.” But that one spray resets the clock. Success comes down to three things:- Starting early - if you act within two weeks of noticing rebound, your success rate jumps to 89%.
- Sticking with corticosteroids - 76% of people who used them consistently got full relief.
- Getting support - talking to a pharmacist or doctor reduces relapse by more than half.
How to Prevent It
The best treatment is prevention:- Never use nasal decongestant sprays for more than 3 days - that’s the official limit now, thanks to FDA labeling rules updated in 2022.
- Try saline rinses first. They’re safe, cheap, and reduce the chance of rebound by 40%.
- Keep sprays out of your medicine cabinet if you’ve had this problem before.
- If you have chronic congestion, see an ENT specialist. You might have allergies, polyps, or a deviated septum - not rebound congestion.
When to See a Doctor
You don’t need to suffer alone. See a doctor if:- You’ve been using nasal spray for more than a week
- Your congestion hasn’t improved after 7 days of stopping
- You’re having trouble sleeping or breathing
- You notice nasal bleeding, crusts, or loss of smell
What’s Next
New treatments are on the horizon. Azelastine nasal spray (an antihistamine) showed 65% effectiveness in early 2023 trials. Low-dose capsaicin is being tested at major hospitals. But for now, the proven path is simple: stop the spray, use steroids, rinse with saltwater, and give your nose time to heal. It’s not easy. But it’s possible. Thousands of people have done it. You can too.Can nasal spray cause permanent damage?
Nasal decongestant sprays don’t usually cause permanent damage if stopped in time. But long-term overuse - especially beyond 6 months - can lead to chronic inflammation, thinning of the nasal lining, and nasal polyps. These can require medical treatment or even surgery. The good news: if you stop the spray early, your nasal tissue typically recovers fully within weeks to months.
Is Flonase safe to use long-term?
Yes. Flonase (fluticasone) and other intranasal corticosteroids are designed for daily, long-term use. Unlike decongestant sprays, they don’t cause rebound congestion. They reduce inflammation and are safe for months or even years when used as directed. Side effects like nosebleeds or dryness are rare and mild.
Why can’t I use oral decongestants instead?
Oral decongestants like pseudoephedrine do reduce nasal swelling, but they work systemically - meaning they affect your whole body. They can raise blood pressure, increase heart rate, and interfere with heart medications. For people with high blood pressure, heart disease, or anxiety, they’re risky. Plus, they don’t treat the inflammation causing the rebound - they just mask it. That’s why doctors recommend nasal steroids instead.
How long does rebound congestion last after stopping the spray?
Symptoms usually peak within 2-3 days after stopping and start improving by day 5-7. Most people feel significantly better by day 10-14. In rare cases, it can take up to 4 weeks, especially if you’ve been using sprays for over a year. Consistent use of nasal steroids and saline rinses speeds up recovery.
Can children get rebound congestion from nasal sprays?
Yes, though it’s less common. Children are more sensitive to the effects of decongestant sprays. The American Academy of Pediatrics advises against using over-the-counter nasal decongestants in kids under 6. If a child has chronic congestion, see a pediatrician - it’s more likely due to allergies, enlarged adenoids, or a structural issue than rebound congestion.
Are there any natural remedies that help?
Saline irrigation is the most effective natural remedy. Steam inhalation, humidifiers, and staying hydrated help too. But essential oils, apple cider vinegar, or herbal drops have no proven benefit for rebound congestion and may irritate your nasal lining. Stick with science-backed methods: saltwater rinses and steroid sprays.