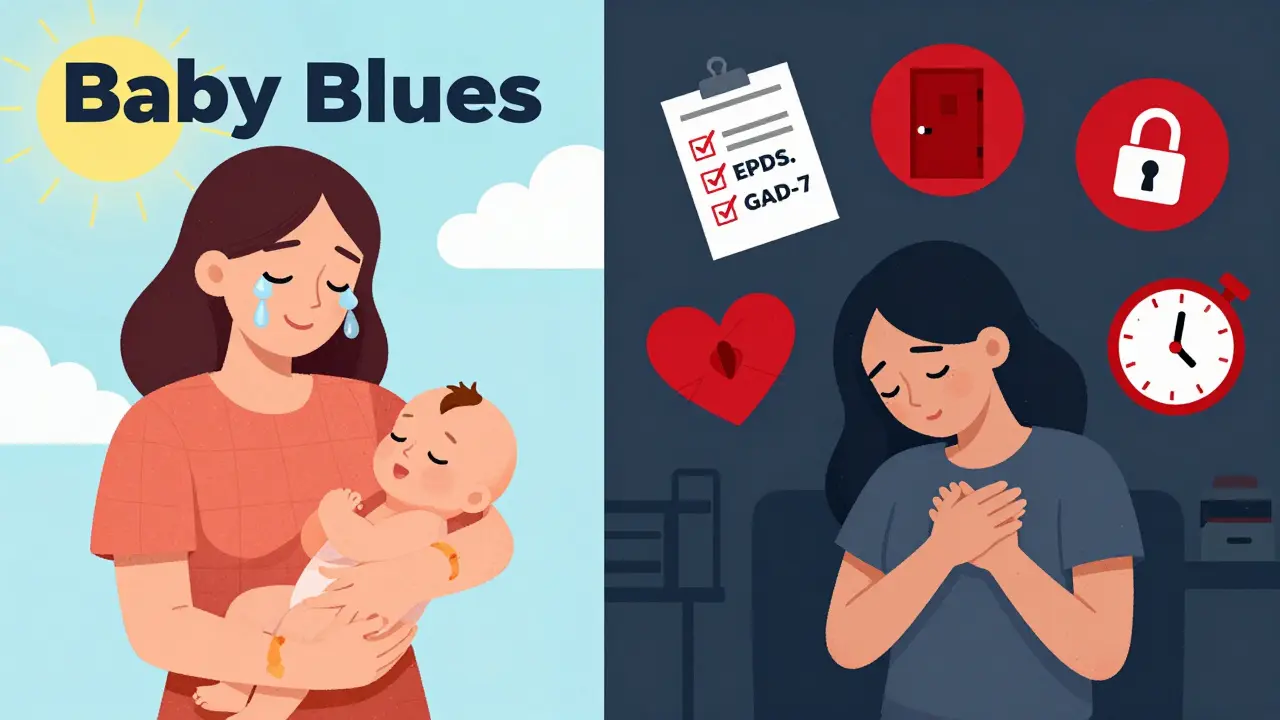
More than 1 in 5 new mothers experience postpartum anxiety - not just stress, not just tiredness, but a deep, persistent wave of worry that doesn’t fade with sleep or time. It’s not the baby blues. Those fleeting tears and mood swings usually vanish within two weeks. Postpartum anxiety sticks around. It keeps you awake when your baby is sleeping. It makes your heart race for no reason. It fills your mind with worst-case scenarios about your child’s safety - even when everything is fine. And too often, it goes unnoticed, dismissed as "just being a new mom."
What Postpartum Anxiety Really Feels Like
Postpartum anxiety isn’t just feeling overwhelmed. It’s a physical and emotional storm. You might feel your chest tighten when your baby cries. You might check on them 10 times an hour, even when they’re breathing normally. You might avoid going out because you’re terrified something will happen to your baby if you’re not right there. Some women report nausea, dizziness, or sudden hot flashes. Others lose their appetite or can’t sleep even when the baby is asleep.
One of the most common - and misunderstood - symptoms is intrusive thoughts. These aren’t signs you’re dangerous. They’re signs your brain is stuck in overdrive. You might picture your baby falling, choking, or getting sick. These thoughts feel horrifying, but they’re not desires - they’re fears amplified by exhaustion and hormones. About 68% of women with postpartum anxiety experience them, compared to just 31% with depression alone.
Physical symptoms are strong indicators. In clinical data, 62% of women report racing heartbeats, 47% feel constant nausea, and 39% lose interest in food. Panic attacks hit 28-35% of cases. These aren’t "normal" new parent worries. They’re persistent, intense, and interfere with daily life - like holding your baby, feeding them, or even showering.
How It’s Different from Baby Blues and Postpartum Depression
Many assume if you’re anxious after birth, you must be depressed. But they’re not the same. Postpartum depression often shows up as sadness, numbness, or guilt. Postpartum anxiety shows up as fear, restlessness, and physical tension.
The Edinburgh Postnatal Depression Scale (EPDS) helps tell them apart. Women with no mental health issues score around 6.2. Those with depression-only score about 11.3. But women with anxiety-only? They average 9.8 - higher than baseline, but lower than depression. When both conditions are present, the score jumps to 14.7. That’s why screening tools need to look beyond just sadness.
Another key difference: duration. Baby blues fade by day 14. Postpartum anxiety lasts weeks or months. If you’re still feeling this way after two weeks, it’s not normal. It’s a signal your body and mind need support.
Who’s Most at Risk?
It’s not random. Certain experiences make postpartum anxiety more likely:
- Having had an anxiety disorder before pregnancy - this raises your risk by 3.2 times
- Experiencing a previous pregnancy loss - 2.7 times higher risk
- Having a baby with medical complications after birth - 2.4 times higher risk
- Having had postpartum depression before - 3.8 times higher risk
It’s not about being "weak" or "overreacting." It’s biology, history, and stress combining in ways your brain isn’t prepared for. If you’ve been through any of these, your risk isn’t theoretical - it’s measurable. And that’s why screening matters.
Screening: Why the EPDS Isn’t Enough Anymore
The Edinburgh Postnatal Depression Scale (EPDS) has been the standard for years. But it wasn’t built to catch anxiety. In fact, it misses up to a third of anxiety-only cases. That’s why in 2023, updated versions now include specific anxiety subscales - questions about panic, racing thoughts, and fear of harm. A multicenter study of over 1,200 women found the new version correctly identified anxiety in 89% of cases.
Another tool gaining traction is the Generalized Anxiety Disorder-7 (GAD-7). It’s shorter, focused, and better at spotting pure anxiety. It has 84% specificity - meaning it rarely mislabels someone as anxious when they’re not. Many clinics now use both tools together: EPDS to catch depression, GAD-7 to catch anxiety.
But here’s the problem: only 67% of U.S. obstetric practices screen routinely. And even when they do, 63% of cases are misdiagnosed as "just stress." That means nearly two out of three women wait an average of 11.3 weeks before getting help. That delay hurts - not just you, but your baby too. Studies show untreated anxiety affects bonding, feeding, and even infant development.
What Works: Care Pathways Based on Severity
Treatment isn’t one-size-fits-all. It’s stepped - based on how bad your symptoms are.
Mild Cases (EPDS 10-12)
For mild anxiety, therapy and lifestyle changes are often enough. Daily 30-minute walks outside reduce anxiety scores by 28% in eight weeks. Yoga and breathing exercises cut symptoms by 33% in clinical trials. Support groups matter too. Women who join new mothers’ groups are 58% more likely to stick with treatment. You’re not alone - and finding others who get it can be healing.
Moderate Cases (EPDS 13-14)
This is where structured therapy becomes essential. Cognitive Behavioral Therapy (CBT) is the gold standard. Twelve to sixteen weekly sessions focused on challenging anxious thoughts, reducing avoidance, and learning grounding techniques show 57% effectiveness in perinatal women. It’s not magic - it’s practice. You learn to notice when your brain spirals, and how to gently pull it back.
CBT alone isn’t always enough for severe cases. But for moderate anxiety, it’s often the first step - and sometimes the only one needed.
Severe Cases (EPDS 15+)
If your anxiety is crippling - if you’re having panic attacks daily, can’t leave the house, or feel like you’re losing control - medication is part of the solution. Selective Serotonin Reuptake Inhibitors (SSRIs) like sertraline are the first-line treatment. Even though they’re not officially "FDA-approved" for postpartum anxiety, decades of research show they’re safe and effective during breastfeeding. Only 0.3% of the maternal dose passes into breastmilk - less than a drop.
Response rates? Around 64% see improvement within eight weeks. But here’s the catch: SSRIs take four to six weeks to work. That’s why doctors pair them with mindfulness training. Daily 10-minute mindfulness practices reduce anxiety symptoms by 41% in just two weeks - giving you relief while the medication kicks in.

What’s New in Treatment
The field is evolving fast. In 2023, the FDA cleared the app MoodMission - a digital CBT tool designed specifically for postpartum women. In a trial of 328 new mothers, users saw a 53% drop in anxiety symptoms after eight weeks. It’s not a replacement for therapy, but it’s a lifeline for those who can’t get to a clinic.
Another promising development: brexanolone (Zulresso). Originally approved for postpartum depression, Phase III trials now show a 72% response rate for anxiety symptoms in just 60 hours - compared to 43% for placebo. It’s not yet approved for anxiety, but it’s under review. If cleared, it could change the game for severe cases.
Insurance coverage has improved too. Since 2021, specific billing codes (CPT 90834 and 90837) exist for postpartum anxiety. That’s raised coverage from 38% to 79% of cases. More women are getting help - but not enough.
The Big Gap: Why So Few Get Help
Here’s the hard truth: only 15% of women with postpartum anxiety get appropriate care. Why?
- Doctors don’t ask the right questions
- Women feel ashamed or guilty for "not enjoying motherhood"
- Therapists trained in perinatal care are scarce, especially in rural areas
- Only 17% of rural hospitals offer specialized programs
It’s not just about treatment. It’s about recognition. As one clinician put it: "Diagnosing postpartum anxiety isn’t about checking boxes - it’s about noticing when someone’s experience is far outside what they consider normal for themselves."
If you’ve been feeling this way, it’s not your fault. It’s not weakness. It’s a medical condition - and it’s treatable. The sooner you speak up, the sooner you can feel like yourself again.
Where to Start
If you’re reading this and thinking, "That’s me," here’s what to do next:
- Take the EPDS and GAD-7 online - they’re free and confidential
- Call your OB, midwife, or pediatrician. Say: "I’ve been feeling really anxious since the baby came. I think I might have postpartum anxiety."
- Ask for a referral to a perinatal therapist or psychiatrist
- Join a support group - even online
- Start small: 10 minutes of deep breathing, a walk around the block, a text to someone who gets it
You don’t have to fix everything today. Just take one step. Your baby needs you - not perfect, not fearless, but present. And you can be present again. Help is out there. You just have to reach for it.
Is postpartum anxiety the same as baby blues?
No. Baby blues are mild mood swings, tearfulness, or irritability that start a few days after birth and usually go away within two weeks. Postpartum anxiety is more intense, lasts longer, and includes physical symptoms like racing heart, panic attacks, and constant worry. It doesn’t fade on its own.
Can I take medication while breastfeeding?
Yes. SSRIs like sertraline are considered safe for breastfeeding. Only about 0.3% of the maternal dose passes into breastmilk - far less than the amount your baby gets from other sources like formula. The benefits of treating your anxiety often outweigh the minimal risk. Always talk to your doctor about options.
How long does postpartum anxiety last?
It can last up to a year if untreated. But with proper care - therapy, lifestyle changes, or medication - most women see significant improvement within 8 to 12 weeks. The key is early intervention. The longer you wait, the harder it becomes to break the cycle.
Are intrusive thoughts dangerous?
No. Intrusive thoughts - like imagining your baby falling or getting sick - are common in postpartum anxiety. They’re not signs you’ll act on them. In fact, the fact that you’re horrified by them means you care deeply. These thoughts are a symptom of anxiety, not a reflection of your character or intentions.
Can my partner help?
Absolutely. Partners can help by listening without judgment, taking over nighttime feedings or diaper changes so you can rest, and encouraging you to seek help. They can even join you in therapy or mindfulness sessions. Support from a partner improves treatment outcomes by up to 40%.
What if I can’t afford therapy?
Many community health centers offer sliding-scale fees. Online platforms like MoodMission and Postpartum Support International provide free or low-cost resources. Some hospitals run free support groups for new mothers. Don’t wait until you can "afford" help - reach out now. Your well-being matters.


Nishant Desae
December 17, 2025 AT 00:26man i just read this and my chest got tight even though i’m not a mom lol. i’ve got a cousin who went through this and no one believed her till she had a panic attack in the grocery store. they thought she was just tired or overreacting. but no, it’s real. the way you described the intrusive thoughts? that’s exactly what she said. she’d stare at the baby in the crib and imagine a fall, and then she’d cry because she felt so guilty for thinking it. but it’s not her fault. it’s her brain being fried from sleepless nights and hormones. we need to stop acting like this is just "mom guilt" and start treating it like the medical thing it is.
Chris Van Horn
December 18, 2025 AT 17:14While I appreciate the clinical rigor of this piece, I must take issue with the uncritical adoption of Western diagnostic frameworks in a global context. The GAD-7, for instance, was developed under a distinctly Anglo-American psychosocial paradigm that pathologizes normal adaptive vigilance in new mothers. In collectivist cultures-such as those in Southeast Asia or Sub-Saharan Africa-maternal hypervigilance is not pathology, but cultural competence. To reduce postpartum anxiety to a checklist of symptoms is not only reductive, it is ethnocentric. Furthermore, the normalization of SSRIs during lactation, while statistically supported, ignores long-term neurodevelopmental data that remains inconclusive. One must ask: Are we healing mothers-or medicating them into compliance?
Virginia Seitz
December 20, 2025 AT 12:30this hit me so hard 😭 i had no idea this was a thing. i thought i was just failing at being a mom. turns out i had anxiety. i cried for an hour after reading this. thank you for writing it. 🙏❤️
Kent Peterson
December 21, 2025 AT 06:21Okay, but let’s be real: this article reads like a pharmaceutical ad disguised as public health advocacy. SSRIs are pushed like candy. Where’s the data on long-term infant exposure? Where’s the discussion on how corporate healthcare incentivizes pill-pushing over therapy? And why is every solution framed as "go to a doctor"? What about community-based support? What about paid parental leave? What about systemic neglect? You’re treating symptoms while ignoring the damn disease: a society that expects women to bounce back from childbirth like it’s a weekend yoga retreat. This isn’t anxiety-it’s capitalism.
Evelyn Vélez Mejía
December 21, 2025 AT 13:47There is a profound metaphysical dimension to postpartum anxiety that this piece, for all its clinical precision, fails to illuminate. The mother, in her new role, becomes a vessel of existential vulnerability-not merely because of hormonal flux, but because she now holds the fate of another life in her trembling hands. The intrusive thoughts are not aberrations; they are the mind’s horrified attempt to simulate every possible catastrophe, a Darwinian hyper-vigilance amplified by the terrifying weight of love. To reduce this to a GAD-7 score is to mistake the tremor for the earthquake. Healing requires not only CBT or sertraline, but ritual, witness, and the sacred recognition that motherhood is not a job-it is a metamorphosis. And metamorphosis is never tidy.
Victoria Rogers
December 23, 2025 AT 06:04so i read this and i’m like… okay cool. but what about the moms who don’t have insurance? or who live in red states where therapists are 2 hours away? or who are undocumented? or who have to work 3 jobs? this whole thing feels like a luxury for white, suburban, college-educated moms. meanwhile, my sister’s neighbor gave birth last week and is still sleeping on the couch because the baby won’t stop crying and her husband’s out working two shifts. nobody’s asking her about EPDS scores. they just hand her a pacifier and say "it’ll pass."
Jane Wei
December 23, 2025 AT 09:33my friend had this after her second kid. she didn’t tell anyone for 6 months. thought she was just "bad at being a mom." then one day she just said, "i think i need help" and everything changed. not because she got meds, but because someone finally said, "that’s not normal, and you’re not alone." just… say it out loud. it helps.
Linda Caldwell
December 25, 2025 AT 01:59you are NOT broken. you are not failing. you are not weak. you are a warrior who just survived the most intense thing a human body can go through-and your mind is trying to protect you, even if it’s doing it in the worst way possible. take a breath. call someone. reach out. you’ve got this. and you’re not alone. i’ve been there. you’re going to be okay. 💪💛
Martin Spedding
December 25, 2025 AT 22:16Typo in the GAD-7 stat. Also, FDA never "cleared" MoodMission-it was 510(k) cleared, which is a regulatory loophole. And the 72% response rate for brexanolone? That’s from a 30-person pilot. Also, why no mention of how postpartum anxiety is overdiagnosed in affluent areas while ignored in poor ones? This article is clickbait dressed as science.
Jessica Salgado
December 26, 2025 AT 22:57the thing no one talks about: what if you don’t want to be a mom? what if you’re anxious because you feel trapped? what if your identity got erased? this article treats motherhood as this sacred, assumed role-but for some of us, the anxiety comes from the loss of self, not the fear of harm. no one asks that question. they just hand you a breathing app and tell you to be grateful. but gratitude doesn’t fix grief.
amanda s
December 28, 2025 AT 13:28As a nurse who’s seen this firsthand, I’m tired of women being told to "just take a walk" or "try yoga." My patient last week had a panic attack while breastfeeding because she thought her milk was poison. She was told to "relax" by her OB. That’s not care-that’s negligence. If you’re having panic attacks, you don’t need a mindfulness app. You need a psychiatrist. Now. And if your doctor won’t refer you? Find another one. Your life matters more than their convenience.
Steven Lavoie
December 29, 2025 AT 01:36My wife went through this after our daughter was born. We didn’t know what it was until she started crying every time she held the baby because she was afraid she’d drop her. We found a perinatal therapist through Postpartum Support International-free, online, and the best thing we ever did. She didn’t need meds. She needed someone to say, "it’s okay to not be okay." And then she needed to know she wasn’t alone. If you’re reading this and you’re scared-reach out. Even if it’s just to a stranger on the internet. You’re not broken. You’re human.