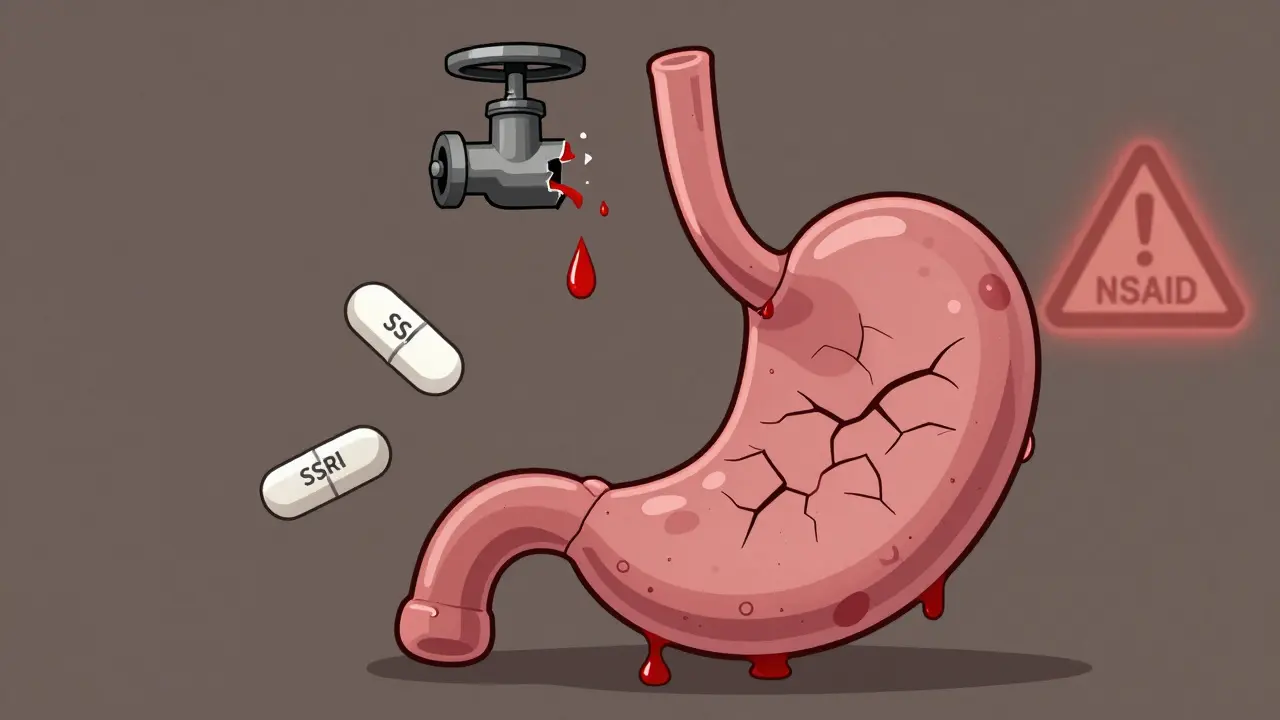
More than 1 in 8 adults in the U.S. takes an SSRI for depression or anxiety. Nearly 1 in 20 takes an NSAID daily for back pain, arthritis, or headaches. What happens when you take both? The answer isn’t just a cautionary note on a prescription label-it’s a real, measurable spike in the chance of life-threatening bleeding in your stomach or intestines.
Why This Combination Is Dangerously Common
SSRIs like sertraline, fluoxetine, and escitalopram are among the most prescribed drugs in the world. NSAIDs like ibuprofen, naproxen, and diclofenac are sold over the counter and in prescriptions, often without a second thought. People take them for years. But when used together, they don’t just add risk-they multiply it.A 2023 meta-analysis confirmed what earlier studies had warned: people taking both an SSRI and an NSAID have a 75% higher risk of upper gastrointestinal bleeding compared to those taking either alone. That’s not a small increase. It’s the difference between a 1 in 100 chance and a 1.75 in 100 chance. For someone over 65 or with a history of ulcers, that’s a 1 in 30 risk over a year. And many patients don’t even know they’re at risk.
The reason isn’t complicated. SSRIs stop platelets from grabbing serotonin, which they need to clump together and stop bleeding. NSAIDs destroy the stomach’s natural protective lining by blocking prostaglandins. Together, they leave you with weak clotting and a damaged stomach wall. It’s like having a broken pipe and no valves to shut it off.
Not All SSRIs or NSAIDs Are Equal
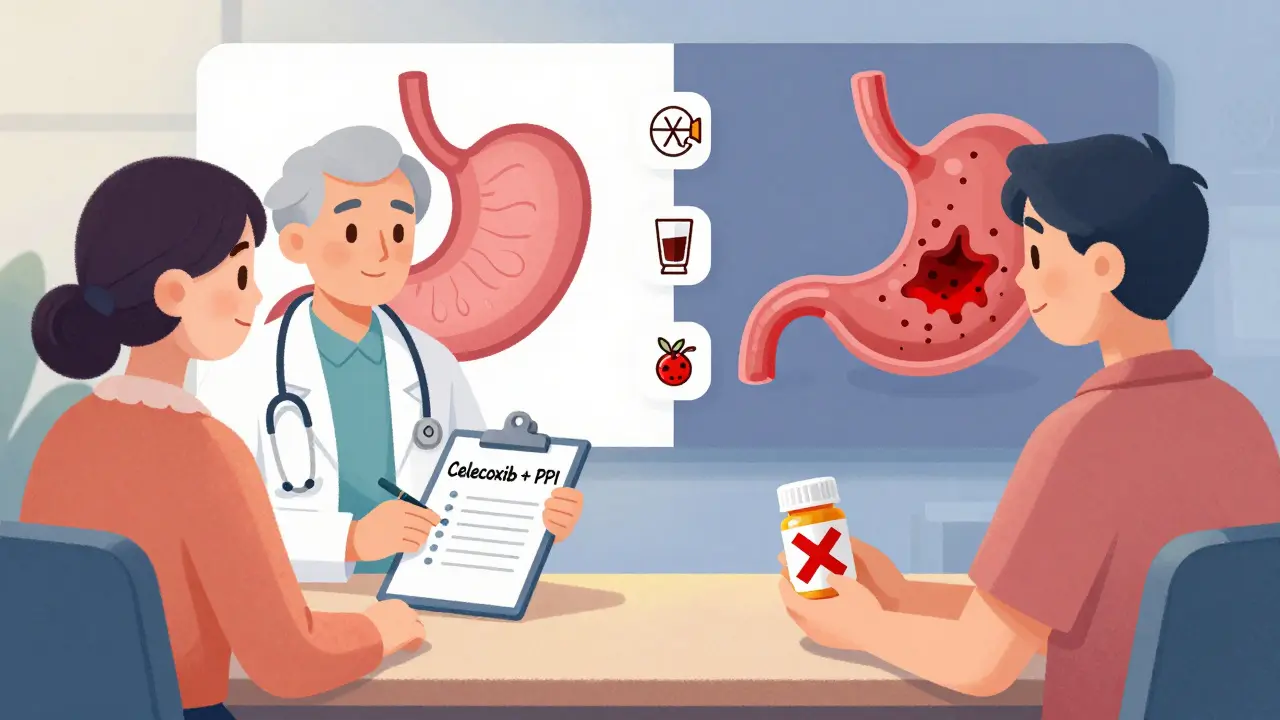
You might assume all SSRIs carry the same risk-and for the most part, they do. But some evidence suggests escitalopram might be slightly less likely to interfere with platelets than paroxetine or fluvoxamine. That’s not a reason to switch without talking to your doctor, but it’s worth noting if you’re already on an SSRI and need pain relief.With NSAIDs, the differences are stark. Ibuprofen carries the lowest GI bleeding risk among non-selective NSAIDs. Naproxen and diclofenac? Much higher. And then there’s celecoxib-a COX-2 inhibitor. Studies show it increases bleeding risk by only about 16% compared to no NSAID use. That’s close to baseline. If you need long-term pain relief and are on an SSRI, celecoxib is the safest NSAID option you can get.
Even aspirin, often thought of as harmless, behaves like an NSAID in this context. If you’re on low-dose aspirin for heart protection and also taking an SSRI, your bleeding risk jumps just as much as it does with ibuprofen. That’s something many cardiologists overlook.
Who’s Most at Risk-and Why
The 75% increased risk sounds scary, but absolute numbers matter more. For a healthy 30-year-old with no history of stomach issues, the chance of bleeding might still be less than 1% per year. But for a 70-year-old with a past ulcer, taking both drugs? Their risk jumps to 5-8% per year. That’s 1 in 12 to 1 in 13 people having a bleed within a year.Other factors stack the deck:
- Age over 65
- History of peptic ulcer or GI bleeding
- Use of corticosteroids or anticoagulants like warfarin
- Helicobacter pylori infection (a common stomach bacteria that causes ulcers)
- Heavy alcohol use
One 2021 study found that nearly 60% of patients hospitalized for GI bleeding from this combination had at least two of these risk factors. Yet, only 22% of them were on a protective medication like a proton pump inhibitor (PPI).
What Doctors Should Be Doing (But Often Aren’t)
A 2021 survey of 1,200 primary care doctors found that only 39% routinely checked for SSRI-NSAID interactions when prescribing either drug. That’s not negligence-it’s ignorance. But it’s ignorance that’s costing lives.The American College of Gastroenterology says clearly: if you’re prescribing an SSRI and your patient is already on an NSAID, or vice versa, you need to either:
- Stop the NSAID and switch to acetaminophen (Tylenol) for pain
- Switch the NSAID to celecoxib
- Add a proton pump inhibitor like omeprazole 20mg daily
And if the patient has any of the risk factors above? You do all three.
But here’s the problem: patients aren’t being told. A 2022 Medscape survey of 452 patients showed 68% said they were never warned about this risk. One Reddit user wrote: “I had black, tarry stools for three days. I thought it was from eating too much spinach. My doctor didn’t mention anything when I started sertraline and kept taking ibuprofen.” He ended up in the ER with a bleeding ulcer.
How to Protect Yourself
If you’re taking both an SSRI and an NSAID right now, here’s what to do:- Don’t panic. But do talk to your doctor or pharmacist. This isn’t an emergency unless you’re vomiting blood or passing black, sticky stools.
- Ask if you really need the NSAID. Can you use acetaminophen instead? For most types of pain-headaches, muscle soreness, joint stiffness-it works just as well without the bleeding risk.
- If you must keep the NSAID, ask for celecoxib. It’s not cheaper, but it’s safer. And if your insurance won’t cover it, ask if they’ll cover a PPI instead.
- If you’re on both, insist on a PPI. Omeprazole 20mg once a day is the standard. Esomeprazole or pantoprazole work too. These drugs are safe for long-term use and reduce your bleeding risk by up to 70%.
- Get tested for H. pylori. If you’ve had ulcers before or are over 50, ask for a breath or stool test. Eradicating this bacteria cuts your risk in half.
One patient on Drugs.com shared: “I switched from naproxen to celecoxib and started omeprazole. Been on this combo for 18 months with zero stomach problems.” That’s the goal.

What’s Changing in 2025
This isn’t a static issue. New tools are emerging:- Electronic health records now flag SSRI-NSAID combos at the prescribing stage. Cleveland Clinic cut hospitalizations for this issue by 42% after adding automated alerts.
- Drugmakers are testing pills that combine NSAIDs with a built-in PPI-like ibuprofen and omeprazole in one capsule. Phase III trials are showing strong results.
- AI models are being trained to predict individual bleeding risk based on age, genetics, lab results, and medication history-with 86% accuracy.
- The FDA and EMA now require warnings on SSRI labels. But warnings don’t prevent use. Education does.
Dr. Amy Foxx-Orenstein, former president of the American College of Gastroenterology, put it bluntly: “We’re approaching a tipping point where prescribing SSRIs and NSAIDs together without protection will be seen as negligent.”
That’s not hyperbole. It’s data.
Bottom Line: You’re Not Alone, But You’re Not Safe
Millions of people are on this combo right now. Most don’t know the risk. And most doctors don’t talk about it.But you do now.
If you’re taking an SSRI and an NSAID, your stomach is under siege. It’s not a myth. It’s not rare. It’s predictable. And it’s preventable.
Don’t wait for black stools. Don’t assume your doctor knows. Ask: “Am I at risk for GI bleeding? Do I need a PPI? Is there a safer painkiller?”
That conversation could save your life.
Can I take Tylenol instead of ibuprofen if I’m on an SSRI?
Yes. Acetaminophen (Tylenol) is the safest pain reliever to use with SSRIs. It doesn’t affect platelets or the stomach lining, so it doesn’t raise bleeding risk. It’s effective for headaches, muscle pain, and arthritis discomfort. Just don’t exceed 3,000 mg per day to avoid liver damage, especially if you drink alcohol or take other medications that affect the liver.
Do all SSRIs increase bleeding risk the same way?
Most SSRIs carry a similar risk because they all block serotonin reuptake in platelets. But some studies suggest escitalopram and sertraline may have slightly lower bleeding risk than fluvoxamine or paroxetine. This difference is small and not enough to justify switching medications unless you’re also at high risk for bleeding. Always consult your doctor before changing antidepressants.
Is celecoxib safe to take with SSRIs?
Celecoxib is the safest NSAID option when used with SSRIs. It doesn’t block COX-1, the enzyme that protects the stomach lining, so it causes far less bleeding risk than ibuprofen or naproxen. Studies show its risk is close to baseline-only about 16% higher than not taking any NSAID. It’s still not risk-free, but it’s the best choice if you need an NSAID long-term while on an SSRI.
Do I need a proton pump inhibitor (PPI) forever if I take both drugs?
Not necessarily. If you stop the NSAID, you can stop the PPI. If you’re on a low-risk NSAID like celecoxib and have no other risk factors, your doctor might reduce the PPI dose or stop it after 3-6 months. But if you’re older, have a history of ulcers, or take other risk-increasing drugs, long-term PPI use is often recommended. PPIs are safe for years in most people and are far safer than a GI bleed.
What are the warning signs of GI bleeding?
Watch for: black, tarry stools (melena), vomiting blood or material that looks like coffee grounds, sudden dizziness or fainting, unexplained fatigue, or severe abdominal pain. These are not normal. If you notice any of these while on SSRIs and NSAIDs, seek medical help immediately. Don’t wait. A GI bleed can become life-threatening within hours.
Can I stop my SSRI if I’m worried about bleeding?
No. Never stop an SSRI suddenly. It can cause withdrawal symptoms like dizziness, anxiety, and even seizures. If you’re concerned about bleeding risk, talk to your doctor about switching to a non-SSRI antidepressant like bupropion, which doesn’t affect platelets. But only make this change under medical supervision.
Is this risk the same in New Zealand and other countries?
Yes. The biological mechanism is the same everywhere. Studies from Europe, Canada, and Australia confirm the same 75% increased risk. New Zealand’s health system follows international guidelines, so the same recommendations apply: avoid combining SSRIs and NSAIDs unless necessary, and always use a PPI if you do. Access to celecoxib or PPIs may vary by prescription policy, but the risk profile doesn’t change.

Diana Alime
December 22, 2025 AT 12:46Ive been on sertraline for 3 years and ibuprofen for my back and nothin happened yet so maybe this is just fearmongering? I dont trust these meta-analyses they always scare people for no reason.
Georgia Brach
December 24, 2025 AT 02:27The 75% increase is statistically significant but clinically misleading. The absolute risk for a healthy individual under 50 remains below 0.5% annually. Framing this as a life-threatening epidemic ignores the baseline probability and induces unnecessary anxiety. Data without context is noise.
Isaac Bonillo Alcaina
December 25, 2025 AT 10:18You people are missing the real issue. This isn't about bleeding risk-it's about the pharmaceutical industry pushing SSRIs like candy while quietly funding studies that downplay NSAID dangers. Celecoxib? That's Pfizer's product. PPIs? AstraZeneca's cash cow. The system is rigged to keep you dependent.
siddharth tiwari
December 26, 2025 AT 12:09in india we dont even have celecoxib easily and ppi are expensive so what do poor people do? doctors just give you paracetamol and say its fine. no one checks for interactions here. we just suffer in silence.
Katie Taylor
December 27, 2025 AT 16:18THIS IS SO IMPORTANT. I almost died from a bleed last year and no one told me. If you’re on an SSRI and taking any painkiller, talk to your doctor TODAY. You’re not being paranoid-you’re being smart. Your gut is worth protecting.
Dan Gaytan
December 27, 2025 AT 19:58Thank you for this. I’ve been on escitalopram and naproxen for 2 years. Just called my pharmacist and switched to celecoxib + omeprazole. Felt like a weight lifted. 🙏
Usha Sundar
December 28, 2025 AT 15:31Black stools? That’s not spinach. That’s your stomach screaming.
Chris Buchanan
December 29, 2025 AT 15:57Wait-you’re telling me I’ve been risking my GI tract for years because I thought Tylenol was ‘weaker’? I’m switching to acetaminophen tomorrow. And yes, I’m asking for the PPI. Thanks for the wake-up call.
Bartholomew Henry Allen
December 31, 2025 AT 10:21Government and pharmaceutical collusion has rendered medical advice meaningless. The FDA’s warnings are symbolic. Real protection comes from personal vigilance and rejecting institutional authority. Your body is your only true physician.
Wilton Holliday
January 1, 2026 AT 21:41Hey, if you're on SSRIs and NSAIDs and haven't talked to your doctor about this yet, don't beat yourself up. Just take one step today-call your pharmacy and ask about celecoxib or PPIs. Progress over perfection. You've got this.
Raja P
January 2, 2026 AT 01:35My uncle had a bleed last year. He was on fluoxetine and naproxen. No warning. Now he’s on tramadol and pantoprazole. He says the pain’s not as gone but he’s alive. This info saved him.
suhani mathur
January 3, 2026 AT 07:02Oh wow. So the ‘safe’ NSAID is celecoxib? Funny how it costs 5x more than ibuprofen. Let me guess-insurance won’t cover it unless you’re over 65 and have three risk factors. Classic. Meanwhile, my 40-year-old neighbor with an ulcer just keeps taking Advil because ‘it works’.
Payson Mattes
January 4, 2026 AT 10:08Did you know the WHO has a secret list of drugs that cause GI bleeds and they’re all patented by Big Pharma? SSRIs and NSAIDs are just the tip. They want you dependent on PPIs so you keep buying them forever. I stopped all meds and now I’m healed with turmeric and cold showers. Just saying.
bharath vinay
January 5, 2026 AT 11:03you think this is bad? wait till you find out SSRIs make you crave sugar and that’s why people get diabetes. NSAIDs are just the distraction. the real enemy is processed food and corporate greed. no one talks about that.
Adarsh Dubey
January 6, 2026 AT 19:25I’ve been on sertraline and ibuprofen for 7 years. No issues. But I also eat well, don’t drink, and got tested for H. pylori last year. Maybe the real takeaway isn’t ‘don’t combine them’ but ‘know your risk factors’. Context matters more than blanket warnings.