Statins and Blood Sugar Risk Calculator
How This Works
Based on clinical studies, we calculate your personalized diabetes risk while taking statins. The calculator factors in your statin type, dosage, and key health factors. Results show your estimated risk percentage over 5 years and provide actionable recommendations to protect your health.
Your Statin Details
Your Health Factors
For millions of people taking statins to lower cholesterol and protect their heart, a quiet concern has grown in recent years: could these life-saving pills also be raising their blood sugar? The answer isn’t simple, but the science is clear - statins can cause a small but real increase in blood sugar levels in some people, pushing a few over the line into type 2 diabetes. It’s not a guarantee, and for most, the heart benefits still far outweigh the risk. But if you’re on statins - or thinking about starting them - you deserve to understand how this works, who’s most at risk, and what you can do about it.
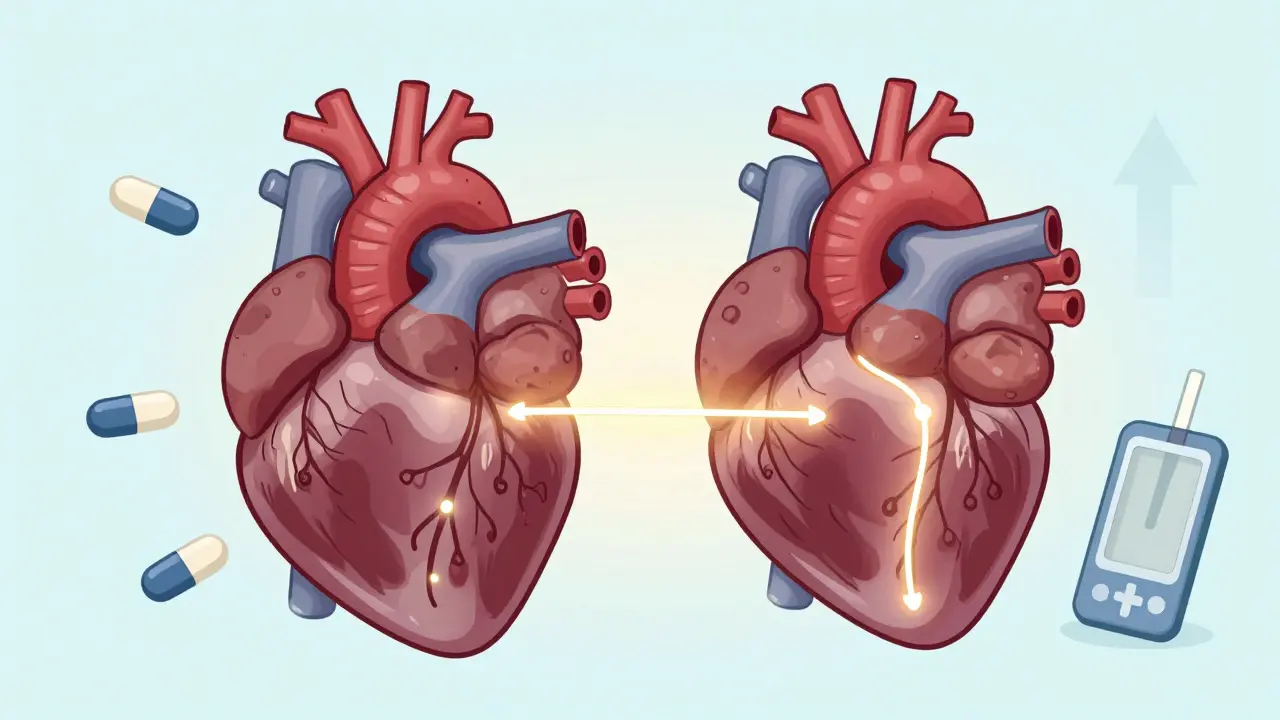
How Statins Affect Blood Sugar
Statins work by blocking an enzyme in your liver that makes cholesterol. But that same enzyme is part of a bigger system called the mevalonate pathway, which also helps produce other important molecules in your body - including those needed for insulin to work properly. When statins slow down this pathway, they reduce levels of substances like geranylgeranyl pyrophosphate and CoQ10. These aren’t just random chemicals; they’re essential for muscle cells and pancreatic beta cells to respond to insulin and release insulin when needed.
Research from the METSIM study, which followed nearly 9,000 people over six years, found that those taking statins had a 46% higher chance of developing type 2 diabetes. Why? Two things happened: insulin sensitivity dropped by 24%, meaning your body didn’t respond as well to insulin, and insulin secretion fell by 12%, meaning your pancreas didn’t pump out as much of it. It’s like your body’s gas pedal and fuel tank both got weaker at the same time.
Another study from Stanford showed that after just 10 weeks on high-dose atorvastatin, insulin resistance went up - and the pancreas tried to compensate by making more insulin. But over time, that compensation fails. That’s when blood sugar starts climbing.
Who’s Most at Risk?
Not everyone on statins develops higher blood sugar. The risk isn’t random - it’s tied to your existing metabolic health. If you already have prediabetes, excess belly fat, high triglycerides, low HDL, or high blood pressure, you’re more vulnerable. These are the same factors that increase your risk of diabetes anyway. Statins don’t create diabetes out of nothing - they nudge people who are already close to the edge over it.
Studies show the risk increases with the dose. People on high-intensity statins - like atorvastatin 40-80 mg or rosuvastatin 20-40 mg - have up to a 36% higher risk of developing diabetes compared to placebo. Those on lower doses, like pravastatin or fluvastatin, have a much smaller increase - around 10%. Age also matters. People over 65 are more likely to see blood sugar changes. And if you’re already diabetic, statins can make your blood sugar harder to control, especially with higher doses.
The Numbers Don’t Lie - But They Don’t Tell the Whole Story
Let’s put the risk in perspective. For every 1,000 people taking statins for five years, about 1 to 2 extra cases of diabetes may occur. That sounds small - and it is. But here’s what that same group gains: roughly 15 fewer heart attacks, strokes, or deaths from heart disease. The American Heart Association says the cardiovascular benefit is about 1.5% over five years. The diabetes risk? Just 0.1% to 0.2% per year.
Think of it like this: if you’re at high risk for a heart attack, skipping statins because you’re worried about diabetes is like refusing a seatbelt because you’re afraid you might get a bruise. The protection is real. But that doesn’t mean you should ignore the bruise.

Which Statins Carry the Highest Risk?
Not all statins are the same when it comes to blood sugar. High-intensity statins - the ones that lower LDL cholesterol the most - also carry the highest diabetes risk:
- Atorvastatin (Lipitor) - Highest risk, especially at 40-80 mg
- Rosuvastatin (Crestor) - Also high risk, especially at 20-40 mg
- Simvastatin (Zocor) - Moderate risk, especially at higher doses
- Pravastatin (Pravachol) - Lowest risk among statins
- Fluvastatin (Lescol) - Also low risk
If you’re at high risk for diabetes - say, you have prediabetes or metabolic syndrome - your doctor might choose a lower-risk statin like pravastatin or fluvastatin, especially if your cholesterol isn’t extremely high. It’s not about avoiding statins. It’s about choosing the right one for your body.
What You Can Do to Protect Yourself
If you’re taking a statin and worried about your blood sugar, here’s what actually works:
- Get tested before and after starting - Ask your doctor for a fasting blood glucose and HbA1c test before you begin statin therapy. Repeat it in 3 to 6 months. If your numbers climb, it’s not necessarily because of the statin - but it’s a signal to pay attention.
- Move more - Just 150 minutes of brisk walking per week can improve insulin sensitivity by up to 25%. Exercise doesn’t just help your heart - it helps your body use insulin better.
- Eat smarter - Cut back on sugar, refined carbs, and processed foods. Focus on vegetables, whole grains, lean protein, and healthy fats. A Mediterranean-style diet has been shown to reduce diabetes risk even in people on statins.
- Watch your weight - Losing just 5-7% of your body weight can cut diabetes risk by more than half. That’s about 10-15 pounds for someone who weighs 200 pounds.
- Don’t stop your statin - If your blood sugar goes up, talk to your doctor. Don’t quit the medication on your own. The risk of a heart attack or stroke is far greater than the risk of developing diabetes.

What About Reversing the Effect?
Some studies suggest that if you stop taking a statin, your blood sugar can return to normal - especially if you’ve only just crossed into prediabetes. But again, this is only under medical supervision. If you have high cholesterol and a history of heart disease, stopping statins could be dangerous.
For people with no prior heart problems but new-onset diabetes after starting statins, switching to a lower-risk statin or lowering the dose may help. In some cases, adding metformin - a common diabetes medication - can offset the insulin resistance caused by statins, without giving up the heart protection.
The Bottom Line
Statins are not the cause of the diabetes epidemic. But for some people, they’re the final nudge that turns prediabetes into full-blown diabetes. The key is knowing your risk and acting on it - not avoiding statins, but managing your health more closely while you take them.
For the vast majority of people who need statins - especially those with high cholesterol, a history of heart disease, or diabetes - the benefits are undeniable. They prevent heart attacks, strokes, and death. But if you’re at risk for diabetes, this is your cue to be proactive. Get tested. Eat well. Move daily. Talk to your doctor. Don’t fear the statin. Use the information to take better care of yourself.
Do statins cause diabetes?
Statins don’t cause diabetes in most people, but they can slightly increase blood sugar levels in some, especially those already at risk. This can push a small number of people with prediabetes over the diagnostic threshold into type 2 diabetes. The risk is real but small - about 0.1% to 0.3% per year of treatment.
Which statins raise blood sugar the most?
High-intensity statins like atorvastatin (Lipitor) and rosuvastatin (Crestor), especially at higher doses (40-80 mg), carry the greatest risk. Lower-intensity statins like pravastatin and fluvastatin have a much smaller effect on blood sugar.
Should I stop taking statins if my blood sugar goes up?
No - never stop statins without talking to your doctor. The risk of heart attack or stroke from stopping is far greater than the risk of developing diabetes. Instead, work with your doctor to adjust your treatment - maybe switch statins, lower the dose, or add lifestyle changes or metformin.
Can lifestyle changes reduce the diabetes risk from statins?
Yes - and this is one of the most powerful tools you have. Regular exercise, losing excess weight, eating fewer refined carbs, and cutting sugar can improve insulin sensitivity and often offset the small rise in blood sugar caused by statins. Many people never develop diabetes even while on statins because they stay active and eat well.
Are there alternatives to statins if I’m worried about diabetes?
For people who can’t tolerate statins or are at very high diabetes risk, alternatives like ezetimibe or PCSK9 inhibitors exist. But they’re usually more expensive and not as effective at reducing heart events. For most people, the best option is still a statin - just chosen carefully and paired with lifestyle changes.

Kipper Pickens
January 24, 2026 AT 18:02Statins inhibit HMG-CoA reductase, which disrupts the mevalonate pathway, leading to reduced geranylgeranylation of proteins critical for insulin vesicle trafficking in pancreatic β-cells. This mechanistic bottleneck impairs glucose-stimulated insulin secretion (GSIS), and when combined with peripheral insulin resistance from adipose tissue inflammation, creates a perfect metabolic storm in predisposed individuals. The METSIM data isn’t noise-it’s a pharmacodynamic signature.
Aurelie L.
January 25, 2026 AT 19:00I got diabetes after my cardiologist pushed me on Lipitor. I didn’t even know I was at risk.