When you hear about tirzepatide for weight loss, it’s not just another diet pill. It’s a scientifically engineered treatment that targets your body’s natural hunger and metabolism systems in ways no single drug has done before. Approved by the FDA for chronic weight management in November 2023 under the brand name Zepbound, tirzepatide isn’t just helping people lose weight-it’s changing how doctors think about obesity treatment.
What Makes Tirzepatide Different?
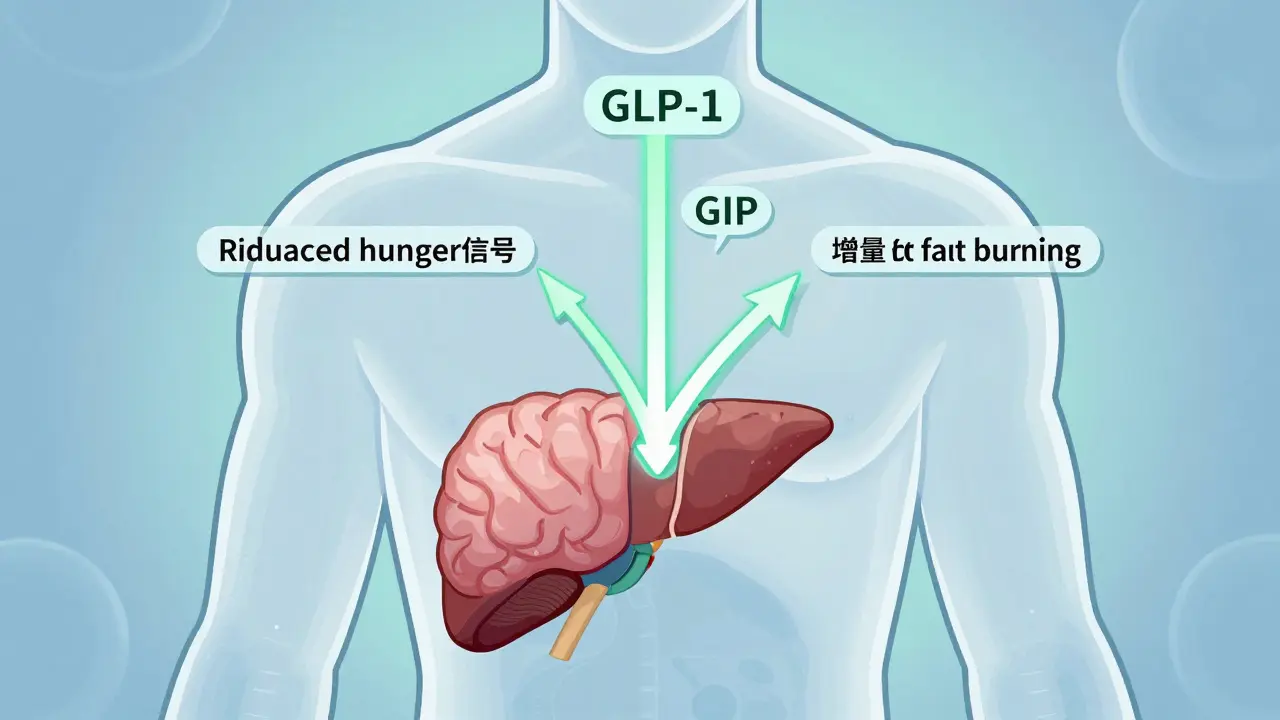
Most weight-loss drugs before tirzepatide worked by mimicking just one hormone: GLP-1. That’s the hormone your gut releases after eating to tell your brain you’re full. Drugs like Wegovy and Saxenda use this single mechanism. Tirzepatide does something new-it activates two receptors at once: GLP-1 and GIP. GIP is another gut hormone that helps regulate insulin and fat storage. Together, they create a combined effect that’s greater than the sum of its parts.This dual action doesn’t just reduce appetite. It also improves how your body uses sugar and fat. Studies show tirzepatide increases insulin sensitivity, reduces fat buildup in the liver, and even boosts energy expenditure. In one major trial, people lost an average of 22.5% of their body weight over 72 weeks on the highest dose (15 mg). That’s more than double the weight loss seen with some older drugs.
How Does It Actually Work in Your Body?
Tirzepatide is a synthetic peptide-a chain of amino acids-that’s designed to last in your system for days. It’s injected once a week under the skin, usually in the belly, thigh, or upper arm. Once it enters your bloodstream, it binds to two types of receptors:- GLP-1 receptors in the brain slow down hunger signals and delay stomach emptying
- GIP receptors in fat tissue and pancreas improve insulin response and help burn fat instead of storing it
Unlike older drugs that mainly made you feel full, tirzepatide also reduces cravings for high-fat, high-sugar foods. People on tirzepatide report less urge to snack, even when they’re not physically hungry. It also lowers levels of ghrelin-the hormone that makes you feel hungry-while increasing adiponectin, a protein that helps your body burn fat more efficiently.
It’s not magic. Your body still needs to adjust. The key is the slow, controlled dosing. You start at 2.5 mg per week and increase every four weeks until you reach your target dose-usually 5 mg, 10 mg, or 15 mg. Rushing the dose increase leads to side effects. Slowing down makes it tolerable.
Real Results: How Much Weight Do People Lose?
The numbers speak for themselves. In the SURMOUNT-1 trial, which included over 2,500 adults with obesity but no diabetes:- People on 5 mg lost 15% of their body weight
- Those on 10 mg lost 19.5%
- At 15 mg, the average was 22.5%
Compare that to semaglutide (Wegovy), the previous gold standard: 14.9% weight loss at the same 72-week mark. Tirzepatide beat it by over 50% in relative terms. That’s not a small difference-it’s life-changing for many.
Real-world data backs this up. On Reddit’s r/Mounjaro community, users report losing 40, 50, even 60 pounds within six months. One person lost 58 pounds on 15 mg without constant hunger pangs. On Drugs.com, 76% of users rated tirzepatide as highly effective for weight loss. That’s rare for any medication.
Side Effects: What to Expect
No treatment is without trade-offs. The most common side effects are gastrointestinal-and they’re real. About 20-25% of people experience nausea, 15-18% get diarrhea, and 7-10% vomit. These aren’t mild. Some users describe them as severe enough to stop treatment.Here’s the catch: most side effects happen during dose escalation. If you jump too fast, your stomach rebels. The FDA-approved schedule stretches over 20 weeks for a reason. Many people who struggled early on say they felt better after slowing down the increases. Some doctors now recommend staying at 5 mg or 10 mg for longer than four weeks if nausea persists.
Other side effects include fatigue, constipation, and dizziness. A small number report gallbladder issues or pancreatitis, but these are rare. The biggest concern is thyroid C-cell tumors seen in rats-but no such link has been found in humans after years of monitoring. Still, if you or a close family member has had medullary thyroid cancer, you shouldn’t take it.
Most people who stop do so because of nausea, not lack of results. But for those who stick with it, the weight loss is often sustained as long as they keep taking it.
What Happens When You Stop?
This is the question no one wants to ask-but you need to know. Tirzepatide doesn’t cure obesity. It manages it. When people stop taking it, weight tends to come back. In follow-up studies, users regained an average of 12-15% of lost weight within six months of stopping.That doesn’t mean it’s useless. Think of it like blood pressure medication. You don’t stop taking it because you feel better-you keep taking it because your body needs the support. For many, tirzepatide gives them the momentum to build lasting habits: better food choices, regular movement, sleep improvements. Those habits can stick even after stopping.
Some doctors now use tirzepatide as a “bridge”-helping patients lose weight fast enough to make lifestyle changes easier. Once they’ve lost 15-20%, they focus on maintenance. A few even cycle on and off under supervision, though this isn’t officially recommended.
Who Should Consider It?
Tirzepatide is approved for adults with obesity (BMI ≥30) or overweight (BMI ≥27) with at least one weight-related condition like high blood pressure, type 2 diabetes, or sleep apnea. It’s not for people who just want to lose a few pounds for a wedding or vacation.It’s also not for everyone. Avoid it if you:
- Have a personal or family history of medullary thyroid cancer
- Have multiple endocrine neoplasia syndrome type 2
- Are pregnant or breastfeeding
- Have severe gastrointestinal disease
People with type 2 diabetes can also use it under the brand name Mounjaro, but Zepbound is the version specifically approved for weight loss. The dosing is the same.
Cost and Access
The list price for a 4-week supply is over $1,000. But that’s not what most people pay. Thanks to manufacturer co-pay programs and insurance, 89% of commercially insured patients pay less than $100 per month. Some pay as little as $45. The Lilly Cares Foundation helps eligible low-income patients get it for free.Insurance coverage varies. Many require proof of failed diet and exercise attempts, or documentation of a weight-related health condition. Medicare doesn’t cover weight-loss drugs yet, but private insurers are increasingly including them. The good news? As more people use it, prices are expected to drop, especially as generics enter the market in the next few years.
What’s Next for Tirzepatide?
In October 2024, the FDA approved Zepbound not just for weight loss-but also for treating obstructive sleep apnea in adults with obesity. That’s huge. It’s the first time a weight-loss drug got approval for a specific condition beyond just shedding pounds.Researchers are now testing tirzepatide for non-alcoholic fatty liver disease (NASH), heart failure, and even Alzheimer’s risk reduction. Eli Lilly is already working on retatrutide, a triple agonist that adds glucagon to the mix. Early results show up to 24.2% weight loss in 24 weeks.
Tirzepatide didn’t just improve weight loss-it opened the door to a new class of drugs. Dual incretin therapy isn’t the end. It’s the beginning.
Getting Started: What to Do Next
If you’re considering tirzepatide:- Talk to your doctor. Bring your BMI, health history, and any previous weight-loss attempts.
- Ask about insurance coverage. Some require prior authorization.
- Be ready to start low and go slow. Don’t rush the dose increases.
- Plan for side effects. Keep ginger tea, crackers, and anti-nausea meds on hand during titration.
- Combine it with lifestyle changes. Exercise and protein-rich meals help reduce side effects and boost results.
This isn’t a quick fix. It’s a tool. And like any tool, its value depends on how you use it.

Rulich Pretorius
December 15, 2025 AT 12:34Tirzepatide’s dual agonism at GLP-1 and GIP receptors represents a paradigm shift in metabolic pharmacology. The GIP component isn’t just additive-it’s synergistic, enhancing insulin sensitivity in adipose tissue while promoting fat oxidation. This isn’t merely appetite suppression; it’s metabolic reprogramming. The SURMOUNT trials demonstrate that the magnitude of weight loss correlates with improved ectopic fat clearance, particularly in the liver. Long-term data still needs to be collected, but the pharmacokinetic profile suggests sustained efficacy with proper titration. The real win? It addresses the neuroendocrine dysregulation at the root of obesity, not just the symptom.
Edward Stevens
December 17, 2025 AT 07:53So we’re paying over a grand a month to feel like a sick squirrel who just ate a whole bag of sour candy? Classic pharma. They turned a hormone into a luxury spa treatment for the overweight rich. Meanwhile, my cousin lost 70 lbs eating rice and doing push-ups in his garage. But sure, let’s keep monetizing biology.
Alexis Wright
December 18, 2025 AT 06:47You people are missing the forest for the insulin spikes. Tirzepatide doesn’t ‘solve’ obesity-it commodifies it. The pharmaceutical-industrial complex needs chronic patients, not cured ones. This drug isn’t medicine; it’s a subscription service for metabolic dependency. And let’s be honest: if you’re taking this, you’re probably still eating processed carbs while pretending you’re ‘doing the work.’ The real solution? Stop eating like a toddler with a credit card. But that’s too simple for a $1,000/month injection.
Daniel Wevik
December 19, 2025 AT 18:34For anyone considering tirzepatide: start at 2.5 mg. Stay there for 6 weeks if you’re even slightly nauseous. Pushing through early side effects doesn’t make you tough-it makes you a statistic. The goal isn’t to hit 15 mg ASAP; it’s to build tolerance so you can stick with it long-term. Pair it with 1.6g/kg of protein daily and resistance training 3x/week. You’ll reduce GI distress and amplify fat loss. This isn’t a magic bullet-it’s a catalyst. You still have to show up.
Rich Robertson
December 20, 2025 AT 19:00As someone who’s watched this drug evolve from lab to living room, I’ve seen it change lives across cultures. In rural Texas, a man lost 80 lbs and got off his CPAP machine. In Detroit, a single mom regained mobility to play with her kids. But it’s not just about weight-it’s about dignity. The stigma around obesity is brutal, and this drug gives people breathing room to rebuild. Just don’t treat it like a shortcut. It’s a tool, not a replacement for self-respect.
Thomas Anderson
December 21, 2025 AT 10:58My aunt tried it. Nausea hit hard at week 2. She dropped to 5mg and stayed there for two months. Lost 30 lbs. No vomiting. Now she’s down 70 total. She still takes it. Doesn’t feel ‘addicted’-feels like she’s just taking her blood pressure med. Simple.
Jonny Moran
December 22, 2025 AT 19:58For those scared of side effects: ginger tea, peppermint oil on wrists, and eating small, bland meals during titration helps more than you think. Also-don’t skip protein. It stabilizes blood sugar and cuts cravings. I’ve seen people quit because they didn’t prep. You wouldn’t run a marathon without training. Same here.
Sinéad Griffin
December 24, 2025 AT 11:41AMERICA NEEDS THIS 🇺🇸💪 No more excuses. If you’re overweight and don’t try this, you’re just lazy. The science is here. The medicine is here. Stop whining about cost-Lilly has programs. Stop complaining about needles-diabetics do it daily. This is the future. Get with it. 🍃💉🔥
Dwayne hiers
December 25, 2025 AT 05:48Regarding the rebound effect post-discontinuation: the 12-15% regain isn’t inevitable-it’s predictable without behavioral scaffolding. The most successful patients in longitudinal studies were those who integrated cognitive behavioral strategies during treatment: mindful eating logs, structured meal timing, and environmental cue modification. Tirzepatide lowers the barrier to change; it doesn’t eliminate the need for it. Think of it as a temporary neuromodulator that buys you time to rewire habits. Without that, yes-you’ll regain. But with it? Many maintain 80% of loss at 2 years. The drug doesn’t fail; the user does-if they treat it as a crutch rather than a catalyst.