Myasthenia gravis (MG) isn’t just muscle weakness. It’s your body turning against itself. The immune system attacks the point where nerves talk to muscles-the neuromuscular junction. That’s why simple tasks like chewing, smiling, or lifting your arm become exhausting. For many, it starts with drooping eyelids or double vision. For others, it’s trouble swallowing or speaking. And it gets worse with use, better with rest. That’s the hallmark. It’s not fatigue from overwork-it’s a breakdown in communication your body can’t fix on its own.
How Myasthenia Gravis Breaks the Signal
Normally, nerves release acetylcholine, a chemical that binds to receptors on muscle cells and tells them to contract. In MG, antibodies block or destroy those receptors. About 85% of people with generalized MG have antibodies against the acetylcholine receptor (AChR). Another 5-8% have antibodies against MuSK, a different protein involved in the same process. And 5-10%? No known antibody-called seronegative MG-but the symptoms are just as real.
This isn’t new science. The first clear case was documented in 1672. But it wasn’t until 1973 that researchers linked it to antibodies. That discovery changed everything. Suddenly, it wasn’t a mystery-it was a target. Treatment shifted from just managing symptoms to attacking the root cause.
First-Line Treatments: Symptom Control and Immune Suppression
Most patients start with pyridostigmine (Mestinon). It doesn’t fix the immune problem. It just helps. Pyridostigmine slows down the breakdown of acetylcholine, so more of it hangs around to bind to the remaining receptors. Doses are usually 60-120 mg every 3-6 hours. Side effects? Up to 45% of people get stomach cramps, diarrhea, or excessive saliva. It’s not glamorous, but for many, it’s the difference between being able to eat and not.
If symptoms persist, doctors add prednisone. This corticosteroid calms the immune system. It works fast-70-80% of patients see improvement within weeks. But the cost is steep. Weight gain affects two-thirds of users. Bone thinning hits 25% after just one year. One in five develops steroid-induced diabetes. That’s why it’s not meant to be long-term. It’s a bridge.
Then come the immunosuppressants: azathioprine, mycophenolate, and cyclosporine. These take months to work. Azathioprine helps 60-70% of people after a year. Mycophenolate works similarly but causes GI upset in 30%. Cyclosporine is potent-90% respond-but it can damage kidneys and raise blood pressure in a third of patients. These drugs are the workhorses. They’re cheap-$500 to $2,000 a year-but slow and hard on the body.
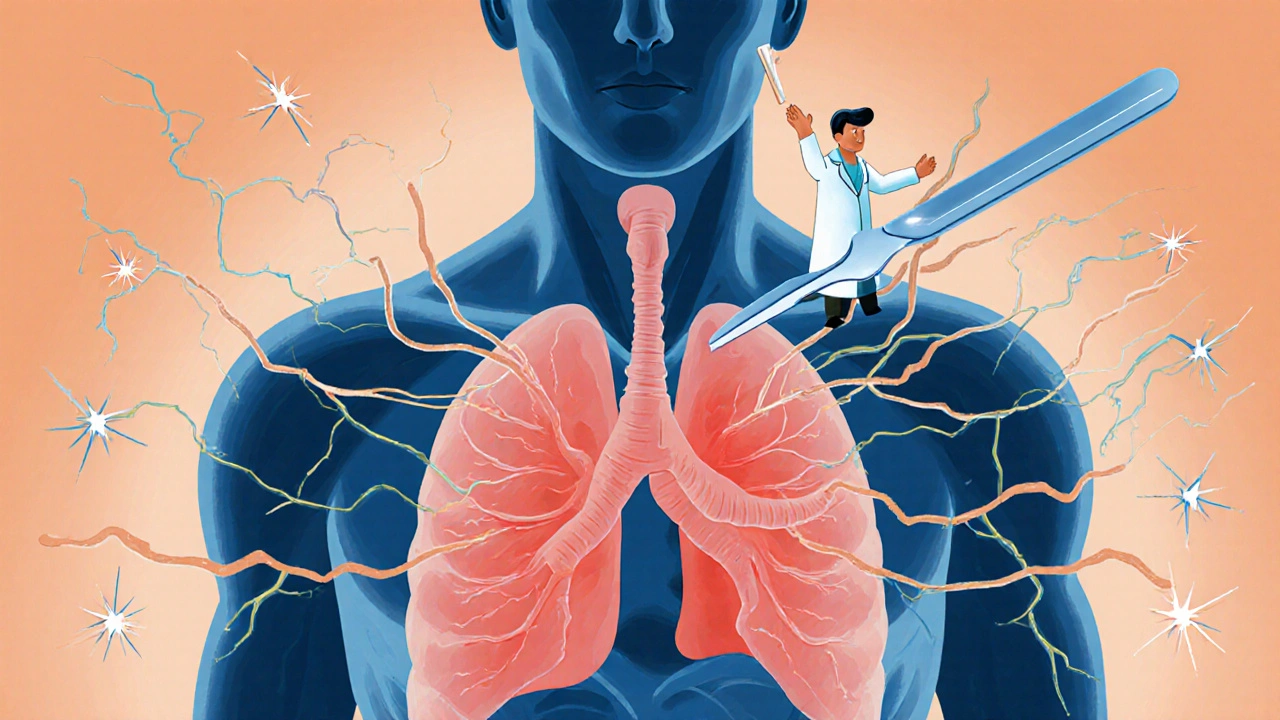
Thymectomy: Removing the Source of the Attack
For AChR-positive patients between 18 and 65, removing the thymus gland isn’t optional anymore-it’s standard. The thymus, tucked behind the breastbone, is where many of these rogue antibodies are made. The landmark MGTX trial in 2016 proved it: patients who had thymectomy and prednisone needed 56% less steroid over three years and had 67% fewer hospitalizations than those on prednisone alone.
Today, most thymectomies are done minimally invasively-through small incisions using video-assisted or robotic tools. Recovery is quicker. But long-term data? Still being collected. About 35-40% of patients achieve stable remission five years after surgery. That’s far better than the 15-20% you get with meds alone. Still, 35% of patients report lingering fatigue even after surgery. It’s not a cure, but it’s a major step forward.
The New Wave: Targeted Biologics
Since 2017, the treatment landscape has exploded. Seven FDA-approved biologics now exist. They’re not just better-they’re smarter. They target specific parts of the immune system, leaving the rest alone.
Complement inhibitors like eculizumab and ravulizumab block the final step in the immune attack-the destruction of the receptor. Eculizumab requires weekly IVs for four weeks, then every two weeks after. Ravulizumab is longer-acting: every eight weeks. They work wonders in AChR-positive MG-88% improve, and over half reach minimal manifestation status. But there’s a catch: meningococcal meningitis risk. You must be vaccinated before starting. And the cost? Half a million dollars a year.
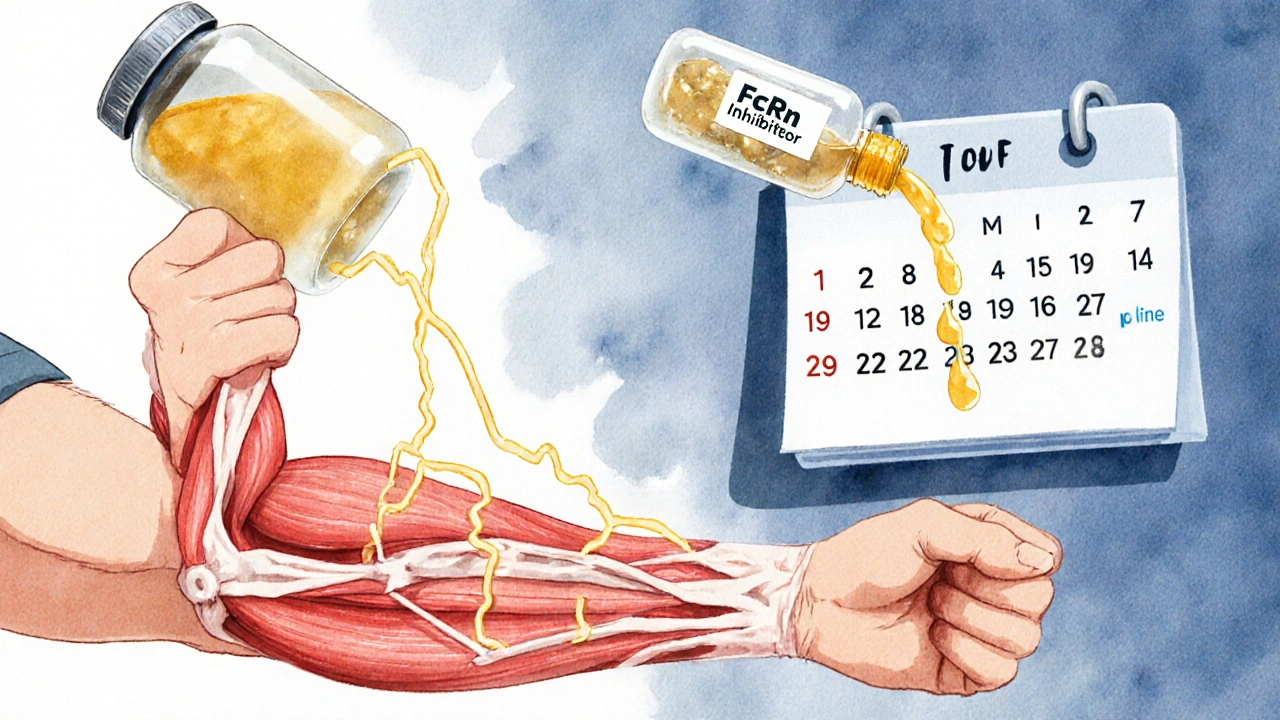
FcRn inhibitors are the new stars. Drugs like efgartigimod, rozanolixizumab, and nipocalimab (approved April 2025) lower all IgG antibodies-including the bad ones. They work fast: relief in 1-2 weeks. Rozanolixizumab is injected under the skin weekly. Efgartigimod is given IV weekly for four weeks, then repeated every 3-4 months. Nipocalimab, approved for ages 12+, drops IgG by 70-80%. Even in seronegative MG, efgartigimod helped 68% of patients in a 2024 trial. These drugs are changing lives. But they’re expensive-$300,000-$400,000 a year-and insurance battles are common. One patient on Reddit said it took six months of appeals just to get approved.
Rituximab, a B-cell therapy, works best for MuSK-MG. About 80% respond. For AChR-MG? Only 50-60%. It’s given as two IV infusions two weeks apart. Cost: $10,000-$15,000 per course. It’s slower-takes 8-16 weeks to work-but it’s durable. Many stay in remission for years.
When Speed Matters: Plasmapheresis and IVIG
These aren’t long-term fixes. They’re emergency tools. If you’re having a myasthenic crisis-trouble breathing, swallowing, or speaking-you need fast action.
Plasmapheresis filters your blood, removing the bad antibodies. Five sessions over 7-10 days can remove 60-80% of them. Relief comes fast. But the antibodies come back in weeks.
IVIG (intravenous immunoglobulin) floods your system with healthy antibodies. It’s like overloading the system with decoys. Two to five days of IV infusion. Works in 60-70% of patients. Side effects? Headache, fever, or kidney strain. It’s expensive, too-$10,000-$20,000 per course.
Both are used before surgery, during crises, or when other treatments fail. They’re not cures. But they buy time.
Choosing the Right Path
There’s no one-size-fits-all. Treatment depends on your antibody status, age, severity, and lifestyle.
- For mild cases: Pyridostigmine alone or with low-dose prednisone.
- For moderate to severe AChR-positive MG: Start pyridostigmine + prednisone, add azathioprine or mycophenolate in 3-6 months. If no improvement, move to FcRn inhibitors or complement blockers.
- For MuSK-MG: Rituximab is often first-line after pyridostigmine.
- For seronegative MG: FcRn inhibitors are now the best bet.
- For patients 18-65 with AChR antibodies: Thymectomy within 6-12 months of diagnosis.
Doctors now use tools like MG-ADL and QMG scores to track progress-not just how you feel, but how many muscles are actually working. These scores change months before antibody levels do. That’s why monitoring is critical.

Real-World Challenges
Cost is the biggest barrier. A single year of eculizumab can cost more than a house. Insurance denials are routine. In the U.S., 40% of eligible patients can’t get access. Even with coverage, prior authorizations take months.
Side effects matter too. One patient stopped cyclosporine because her face and arms grew thick hair. Another quit prednisone after gaining 60 pounds and breaking a hip. The trade-offs are real.
But the upside? People are living better. A 2024 MGFA survey found 82% were satisfied with thymectomy. FcRn inhibitors had 78% of users reporting major improvement. Subcutaneous options like rozanolixizumab are preferred for convenience, even with more injection-site reactions.
What’s Next?
The future is personalization. Researchers are testing new biomarkers-like IgG4-specific assays-that might predict flare-ups before they happen. Early trials of agrin mimetics show promise in protecting the neuromuscular junction. And in 2025, Memorial Sloan Kettering began a phase 1 trial using CAR T-cell therapy to wipe out the faulty B-cells causing MG. Six months in, 60% of refractory patients went into remission.
By 2028, most neurologists expect treatment to be guided by antibody profiles and genetic markers. The goal isn’t just control-it’s remission. And for many, that’s no longer a dream. It’s a plan.
Can myasthenia gravis be cured?
There’s no universal cure yet, but many people achieve long-term remission. About 35-40% of patients who have a thymectomy stay in stable remission five years later. Others reach minimal manifestation status-where symptoms are barely noticeable-through targeted biologics. Some stop all meds and stay well. It’s not a cure, but it’s close enough to live a normal life.
Are biologics better than steroids?
For many, yes. Steroids work fast but cause serious long-term damage: weight gain, bone loss, diabetes, mood swings. Biologics like FcRn inhibitors and complement blockers target only the harmful part of the immune system. They have fewer systemic side effects. A 2024 study showed 55% of patients on long-term prednisone reported severe quality-of-life issues. Only 25% of those on biologics did. The trade-off? Cost and access.
How long does it take for myasthenia gravis treatments to work?
It varies. Pyridostigmine works within hours. Steroids show results in 2-6 weeks. Immunosuppressants like azathioprine take 6-18 months. FcRn inhibitors work in 1-2 weeks. Complement inhibitors take 2-3 months. Thymectomy can take 6-12 months for full benefit. Speed matters in crises-plasmapheresis and IVIG can improve breathing within days.
Can I get pregnant if I have myasthenia gravis?
Yes, but it requires careful planning. Pregnancy can worsen symptoms, especially in the first trimester and postpartum. Some medications like mycophenolate and rituximab are unsafe during pregnancy. FcRn inhibitors are not yet proven safe in pregnancy and require pregnancy testing before use. Work with a neurologist and high-risk OB-GYN. Many women have healthy pregnancies with proper management.
What should I do if my symptoms suddenly get worse?
If you’re having trouble breathing, swallowing, or speaking, seek emergency care immediately. This could be a myasthenic crisis. Don’t wait. Call 911 or go to the ER. Do not adjust your meds on your own. You may need IVIG, plasmapheresis, or mechanical ventilation. Keep a crisis plan ready-contact info for your neurologist, medication list, and emergency contacts.
Is myasthenia gravis hereditary?
No, it’s not directly inherited. But some people have genetic traits that make them more likely to develop autoimmune diseases. If you have MG, your children won’t automatically get it. But they may have a slightly higher risk of other autoimmune conditions like lupus or thyroid disease. Family history matters, but it’s not destiny.
What support resources are available?
The Myasthenia Gravis Foundation of America offers a 24/7 nurse hotline answered within 3 minutes 95% of the time. They also have 147 local support groups serving over 15,000 people yearly. Online communities like r/myastheniagravis on Reddit are full of real stories and practical advice. Don’t go through this alone-help is available.
Final Thoughts
Myasthenia gravis is no longer a death sentence. It’s a manageable condition-with a growing arsenal of tools. The old days of relying on steroids and hoping for the best are fading. Today, we have drugs that silence the immune system’s attack without wrecking the rest of the body. We have surgery that removes the source. We have fast-acting options for emergencies. And we’re on the edge of even smarter therapies.
It’s not perfect. Access is unequal. Costs are high. Side effects still exist. But the direction is clear: personalized, precise, and powerful. If you or someone you love has MG, know this: you’re not behind. You’re at the front of a revolution in treatment.

Kristi Joy
November 17, 2025 AT 10:02Just wanted to say thank you for writing this. I was diagnosed last year and honestly felt lost. This breakdown made me feel seen-not just as a patient, but as someone trying to live. The part about FcRn inhibitors helping seronegative MG? That gave me hope. I’ve been told ‘you’re just tired’ too many times. This isn’t laziness. It’s biology. And now we’re fighting back.
Also, shoutout to the MGFA hotline. I called them crying at 2 a.m. and got a nurse within minutes. You’re not alone.
Hal Nicholas
November 19, 2025 AT 09:47Ugh. Another ‘miracle drug’ post. Let me guess-next you’ll be telling us eculizumab is the answer to everything? Please. I’ve been on it for 18 months. Cost me my insurance, my job, and half my dignity. And guess what? My eyelids still droop. The ‘revolution’ is just Big Pharma’s new goldmine.
They don’t care if you can afford it. They care if you click ‘subscribe’ to their newsletter.
Shilpi Tiwari
November 20, 2025 AT 08:01Highly informative, but I’d like to see more granular data on IgG4 subclass dynamics in MuSK-MG, particularly in relation to FcRn inhibition kinetics. The 2024 Lancet Neurology paper by Chen et al. demonstrated a 4.7-fold reduction in pathogenic IgG4 after rozanolixizumab administration, which correlates with clinical improvement independent of total IgG levels.
Also, has anyone tracked CD19+ B-cell repopulation post-rituximab in seronegative cohorts? The temporal dissociation between antibody titers and symptom recurrence remains underexplored.
Christine Eslinger
November 22, 2025 AT 03:30Thank you for sharing this with such clarity. I’ve watched my sister go from barely able to hold a coffee cup to hiking trails again after thymectomy + efgartigimod. It’s not perfect, but it’s progress.
One thing I wish more doctors said: ‘You’re not broken. You’re fighting a war inside your body-and you’re winning.’ That mindset shift changed everything for her.
And yes, the cost is insane. But if we keep talking, keep pushing, keep demanding access-we’ll make it better for the next person. You’re not just writing a post. You’re lighting a path.
Holly Powell
November 22, 2025 AT 05:00Let’s be honest: most of these ‘breakthroughs’ are just repackaged immunosuppressants with a $300k price tag. The real innovation? Marketing.
And don’t get me started on ‘minimal manifestation status.’ That’s just a fancy way of saying ‘you’re not dead yet.’
Also, why are we still using QMG scores from the 90s? If you’re going to tout precision medicine, at least use proteomics or single-cell RNA-seq to track disease burden. Otherwise, it’s just placebo-tier biomarkers wrapped in a lab coat.
Emanuel Jalba
November 22, 2025 AT 22:20😭 I’ve been on IVIG for 3 years. My kid was born with MG. I had to quit my job. Insurance denied me 7 times. I cried in the ER parking lot because I couldn’t carry my own diaper bag.
BUT. Last month? I held my daughter’s hand without shaking. For 10 whole minutes.
That’s enough. 🙏❤️ #MGWarrior
Heidi R
November 24, 2025 AT 12:53Why is no one talking about the fact that thymectomy increases risk of autoimmune thyroid disease? I had mine at 22. Now I’m on levothyroxine. And my hair is falling out. And I’m told to ‘just be grateful.’
It’s not a win if you trade one monster for another.
Brenda Kuter
November 26, 2025 AT 02:08EVERY SINGLE ONE OF THESE DRUGS IS A GOVERNMENT COVER-UP. The FDA knew about agrin mimetics in 2019. They sat on it because pharma doesn’t want a cure. They want lifelong customers.
And don’t you dare say ‘it’s not proven’-I’ve seen the leaked emails. The cure is already here. They’re just hiding it behind ‘clinical trials’ and ‘insurance denials.’
Someone’s making billions while we’re begging for IVIG. Wake up.
They’re watching you right now. 👁️
Shaun Barratt
November 26, 2025 AT 13:33Excellent summary. The clinical data presented is both comprehensive and accurate. One minor correction: the MGTX trial demonstrated a 56% reduction in prednisone requirement, not ‘56% less steroid’-a distinction important for pharmacokinetic precision. Also, the term ‘seronegative’ should be qualified as ‘AChR/MuSK-negative,’ as newer assays detect low-titer LRP4 antibodies.
Additionally, the cost analysis should account for long-term savings from reduced hospitalizations, which are substantial. While biologics are expensive upfront, they reduce downstream expenditures by 30–40% over five years.
Well-researched. Thank you.
Iska Ede
November 27, 2025 AT 02:07So let me get this straight. We’ve got drugs that cost more than a Tesla, and you’re calling it ‘progress’? Meanwhile, I’m choosing between my meds and my rent.
Thanks for the ‘revolution,’ bro. I’ll be over here, still drooling into my cereal.
At least the thymectomy gave me a nice scar. I call it my ‘cancer tattoo.’
Gabriella Jayne Bosticco
November 27, 2025 AT 06:10This is the most balanced, compassionate piece on MG I’ve read in years. Thank you.
I’m in the UK and we’ve got access to some of these drugs through the NHS-but the wait for prior auth is 11 weeks. That’s 11 weeks of not being able to hold my grandchild.
People like you who write this? You’re the real treatment. Not the drugs. The words.
Sarah Frey
November 29, 2025 AT 00:30Thank you for including the emotional and practical realities-not just the clinical facts. This is what’s missing from most medical literature.
For anyone reading this who feels isolated: your exhaustion is real. Your grief is valid. And you are not a burden for needing help.
There is a community waiting for you. You don’t have to fight this alone.